Palmoplantar psoriasis (PP) is a localized variant of psoriasis1 whose prevalence in children ranges from 1.6% up to 18.5%.2 PP can appear in isolation or as a sign of psoriasis in other areas of the body. PP can be categorized into 3 main clinical types: palmoplantar plaque psoriasis, palmoplantar pustulosis, and continuous acrodermatitis of Hallopeau.2 Lesions are characterized by well-demarcated erythematous plaques with thick, white-yellow scales.3 They may also be accompanied by extracutaneous signs, such as nail changes and arthritis in affected fingers.3
Although the affected body surface area is typically small, as it is localized mainly on the palms and soles, PP is considered a severe clinical variant. Fissures, tissue hardening, and hyperkeratosis significantly impact everyday activities and are challenging to treat.4 The objective of the study was to describe the clinical–epidemiological aspects and treatment of PP in children.
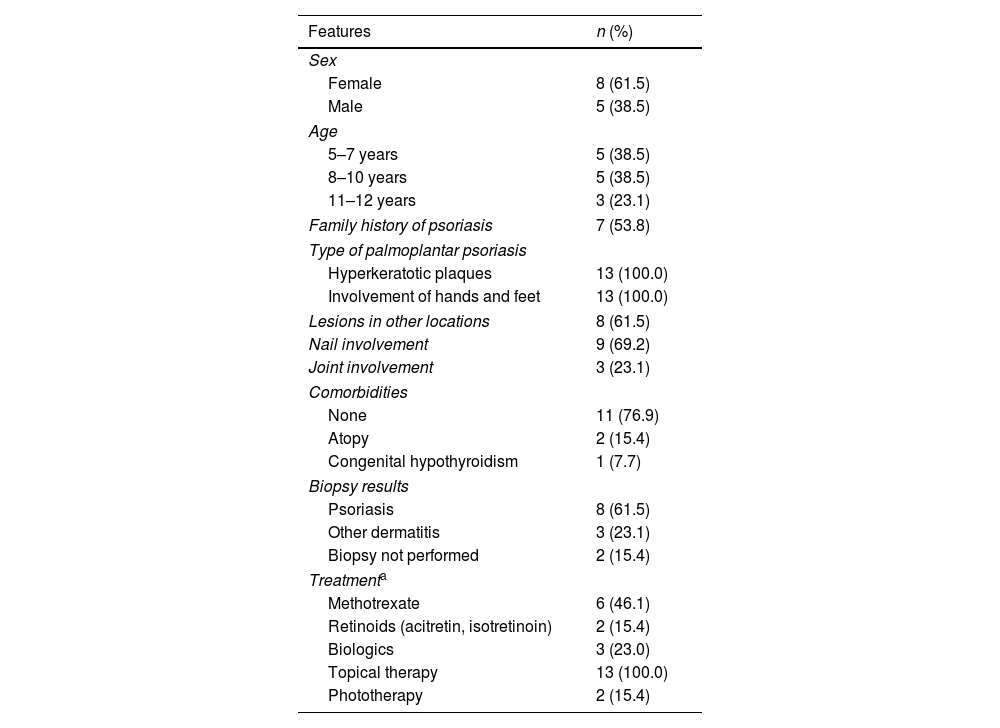
We conducted a retrospective study by reviewing the health records of pediatric patients diagnosed with PP seen in outpatient consultations from January 2001 through February 2022 at Hospital Ramos Mejía and Hospital Aleman (Buenos Aires, Argentina). A total of 13 patients were included whose median age was 7.7 years (range, 5–12 years). The mean time since diagnosis was 1.5 years, and it was more common in females (Table 1). Seven patients had a family history of psoriasis. All exhibited the hyperkeratotic plaque variant with bilateral and symmetrical involvement of palms and soles (Fig. 1). Eight patients exhibited lesions in other locations, such as extremities, scalp, and genital areas. Nail changes—such as pitting, discoloration, longitudinal ridges, dystrophy, and onycholysis—were found in 9 patients. A total of 11 patients required histopathological studies, which confirmed psoriasis in 8 cases and described nonspecific dermatitis in 3. In the remaining 2 cases, biopsy was not required due to characteristic clinical diagnosis and lesions in other locations. Initial treatment for all was topical, but due to lack of clinical improvement, alternative treatments such as methotrexate, acitretin, and isotretinoin were used (Table 1). Only 3 patients who did not improve with previous treatments required biologics (1 with infliximab and 2 with etanercept), while 2 underwent phototherapy along with methotrexate (1) or topical therapy (1).
Characteristics of pediatric patients with palmoplantar psoriasis in Argentina.
| Features | n (%) |
|---|---|
| Sex | |
| Female | 8 (61.5) |
| Male | 5 (38.5) |
| Age | |
| 5–7 years | 5 (38.5) |
| 8–10 years | 5 (38.5) |
| 11–12 years | 3 (23.1) |
| Family history of psoriasis | 7 (53.8) |
| Type of palmoplantar psoriasis | |
| Hyperkeratotic plaques | 13 (100.0) |
| Involvement of hands and feet | 13 (100.0) |
| Lesions in other locations | 8 (61.5) |
| Nail involvement | 9 (69.2) |
| Joint involvement | 3 (23.1) |
| Comorbidities | |
| None | 11 (76.9) |
| Atopy | 2 (15.4) |
| Congenital hypothyroidism | 1 (7.7) |
| Biopsy results | |
| Psoriasis | 8 (61.5) |
| Other dermatitis | 3 (23.1) |
| Biopsy not performed | 2 (15.4) |
| Treatmenta | |
| Methotrexate | 6 (46.1) |
| Retinoids (acitretin, isotretinoin) | 2 (15.4) |
| Biologics | 3 (23.0) |
| Topical therapy | 13 (100.0) |
| Phototherapy | 2 (15.4) |
(A) Erythematous–squamous plaque with hemorrhagic crusts and fissures on the palms and fingers of both hands. (B) White-yellowish keratotic plaques on the soles and toes of both feet, with fissures and hemorrhagic crusts. (C) White-yellowish keratotic plaques on the soles extending to the toes, with the presence of fissures. (D) Whitish keratotic plaques on the palms and fingers, with fissures and hemorrhagic crusts. (E) Erythematous-desquamative plaque on the distal region of the first finger of the left hand, with fissures and periungual and nail involvement (discoloration, longitudinal ridges, pitting, and nail dystrophy).
In our study, more than half of the patients exhibited nail involvement, higher than the 31% reported in a different study,5 which may be explained by distal finger involvement extending to periungual areas, leading to changes from dystrophy to complete nail detachment.4 Nail involvement has been the most important clinical predictor of psoriatic arthritis in adult patients6; however, no studies have ever linked this relationship in children, and in our series, only 3 patients had confirmed joint involvement with radiological changes.
Common severity staging scales, such as the Psoriasis Area and Severity Index (PASI) or the Body Surface Area (BSA), have limited utility when psoriasis is restricted to hands and feet. According to these scales, severity would never be greater than mild (BSA<5%); however, significant functional impairment warrants considering PP as severe.7 Amode et al. described PP as severe when phototherapy or systemic treatment was required.2 For this reason, specific scales such as the Palmoplantar Psoriasis Area and Severity Index (PPPASI) exist but are rarely used in the routine clinical practice. In our series, only 1 patient received exclusively topical therapy, demonstrating the trend to consider PP as moderate-to-severe in most patients, even if PASI and BSA are low, due to functional impairment, pain, and esthetic concerns, which are highly significant in this population.
Currently, there are no specific treatment guidelines for the management of this psoriasis variant in pediatric populations. Therapeutics are decided based on disease extent, duration, and functional impairment.
In conclusion, P was more common in females and in those with a family history of psoriasis. The first-line therapy used was topical, followed by methotrexate or retinoids, due to disease severity. Only 3 patients required biologics. It is crucial to consider PP as a severe variant, even in this population, and understand the necessity of treatment aligned with severity to avoid delays and promote patient improvement.
Authors’ contributionsAll authors participated in the study design. All contributed to data acquisition and manuscript drafting and approved the final version. PCL and RAPC: study conception and design, data collection and analysis, manuscript drafting, critical manuscript review, and final approval. MEA, AA, NAA, and ML: data collection and analysis, critical manuscript review, and final approval. All authors are accountable for all aspects of the manuscript.
FundingThis study was self-funded.
Conflicts of interestNone declared.