Complete surgical excision is the most common treatment for basal cell carcinoma (BCC), and this intervention is often performed by surgeons who are not dermatologists (e.g., plastic surgeons, general surgeons, oral and maxillofacial surgeons, ophthalmologists, and otorhinolaryngologists).
ObjectivesTo determine positive margin rates in BCCs removed by surgeons from different specialties and to identify clinical and pathologic factors that might explain potential differences between specialties.
MethodsWe retrospectively reviewed the pathology reports of all BCCs diagnosed at Hospital Universitari Vall d’Hebron between January 2009 and March 2001. The statistical methods included a descriptive analysis of clinical and pathologic variables, standard statistical analyses, and multivariate logistic regression.
ResultsWe included 921 BCCs from 750 patients; 549 of the tumors had been excised by a dermatologist. The overall positive margin rate was 12.6%, but the rate for tumors removed by dermatologists was significantly lower than that for those removed by other specialists (6.7% vs 21.5%). There was a 3.8-fold increased relative risk of positive margins following excision by a surgeon who was not a dermatologist, independently of patient age, tumor site, maximum diameter of the resected specimen, and histologic subtype.
ConclusionsAccurate macroscopic identification of tumor margins, which are often difficult to see, and familiarity with the natural history of BCC are key factors in the successful surgical treatment of BCCs. The higher rate of tumor-free margins achieved by dermatologists in this study is probably mainly due to their greater experience in these 2 areas.
El tratamiento más utilizado para el carcinoma basocelular (CBC) es la extirpación quirúrgica completa, que en muchas ocasiones es realizada por facultativos no dermatólogos (cirujanos plásticos, cirujanos generales, cirujanos maxilofaciales, oftalmólogos y otorrinolaringólogos).
ObjetivosDeterminar la prevalencia de márgenes quirúrgicos afectados por el CBC en función del especialista que lo interviene e identificar parámetros clínico-patológicos que puedan justificar las potenciales diferencias en estas prevalencias.
MétodosEstudio retrospectivo de los informes histológicos con diagnóstico de CBC del Hospital Universitari Vall d’Hebron entre enero de 2009 y marzo de 2010, con análisis descriptivo de las características clínico-patológicas y análisis estadístico y multivariable mediante regresión logística.
ResultadosSe incluyeron 921 tumores de 750 pacientes. Los dermatólogos extirparon 549 lesiones. Los márgenes de la pieza quirúrgica estaban invadidos por el tumor en un 12,6% de las lesiones. La extirpación fue incompleta en un porcentaje significativamente menor de tumores intervenidos por dermatólogos frente a otros especialistas (6,7 vs 21,5%). El riesgo relativo de que queden márgenes afectados es 3,8 veces mayor si el cirujano no es dermatólogo, independientemente de la edad del paciente, la localización de la lesión, el diámetro máximo de la pieza extirpada y el subtipo histológico del tumor.
ConclusionesLa correcta identificación macroscópica de los márgenes tumorales, muchas veces sutiles, y el conocimiento de la historia natural del CBC son claves para un adecuado abordaje quirúrgico; probablemente son los principales factores que justifican el mayor porcentaje de tumores con márgenes libres extirpados por los dermatólogos.
Basal cell carcinoma (BCC) is the most common malignant tumor in humans, second in frequency only to actinic keratosis if squamous cell carcinoma in situ is also taken into consideration. Numerous studies have pointed to a rise in the incidence of BCC in the last 2 decades.1
Eighty-five percent of BCCs are located on the face and neck.2 These slow-growing tumors have a very low metastatic potential, but without correct management they can be locally destructive, particularly on the face. Infiltrative tumors usually display an irregular pattern of growth and their depth may not be evident on visual inspection or palpation.3,4
The treatment approach can be chosen on the basis of various factors, such as the treating physician's experience, patient preferences and characteristics (age, concomitant conditions), tumor location and size, histologic subtype, and previous treatments. The treatment most commonly used with intention to cure is surgical excision, usually with predetermined margins ranging in breadth between 2 and 15mm. Margins of 4mm have been recommended by Thomas and coworkers5 for BCCs of less than 20mm, but only 7% of small, well-circumscribed BCCs have been found to have invaded tissue more than 1mm beyond the clinically visible tumor margin.6 When Gulleth and coworkers2 retrieved 973 articles describing 10 066 BCCs (PubMed) for meta-analysis, they concluded that a margin of 3mm is adequate to achieve a 95% cure rate when nonmorpheaform BCCs of up to 2cm in diameter are excised. Other treatments available for these tumors include topical imiquimod, cryotherapy, curettage, photodynamic therapy, radiotherapy, and Mohs micrographic surgery. The Mohs technique evaluates all surgical margins around the excised tumor during the intervention itself or afterwards (deferred Mohs technique) and it is this procedure that achieves the highest cure rates. Mohs surgery is not available in all hospitals, however, is costly, and is reserved for selected cases.
To attain a cure by oncologic surgery, tumors must be classified by type and their borders identified macroscopically, with care to avoid leaving residual tumor that would make additional operations or other treatments necessary. In this study we aimed to determine whether surgical specialty influences the ability to excise margins that are microscopically free of tumor cells. A secondary aim was to assess the influence of such factors as age, tumor location and size, and histologic subtype on the results achieved by surgeons from different specialties.
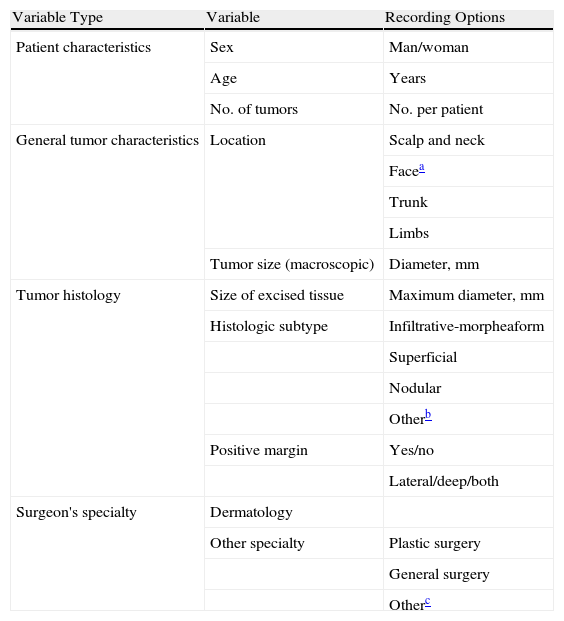
Patients and MethodsWe retrospectively reviewed all pathology reports with a histologic diagnosis of BCC in the records of Hospital Universitari Vall d’Hebron in Barcelona from January 1, 2009, to March 31, 2010. Biopsies performed without intention to completely excise the tumor and those treated by physicians who were not members of our hospital or community specialist outpatient clinic staffs were excluded in an effort to avoid introducing possible bias stemming from the care setting or the surgeons’ skills and expertise. None of the excisions included in the study were done by Mohs micrographic surgery. Data collected are summarized in Table 1.
Data Extracted for Analysis From Pathology Reports for Tumors With a Histologic Diagnosis of Basal Cell Carcinoma.
| Variable Type | Variable | Recording Options |
| Patient characteristics | Sex | Man/woman |
| Age | Years | |
| No. of tumors | No. per patient | |
| General tumor characteristics | Location | Scalp and neck |
| Facea | ||
| Trunk | ||
| Limbs | ||
| Tumor size (macroscopic) | Diameter, mm | |
| Tumor histology | Size of excised tissue | Maximum diameter, mm |
| Histologic subtype | Infiltrative-morpheaform | |
| Superficial | ||
| Nodular | ||
| Otherb | ||
| Positive margin | Yes/no | |
| Lateral/deep/both | ||
| Surgeon's specialty | Dermatology | |
| Other specialty | Plastic surgery | |
| General surgery | ||
| Otherc |
Descriptive statistics were compiled for demographic variables as well as for the clinical and histologic characteristics of the tumor and the specialties of the surgeons who performed the excisions. Statistics were analyzed for the group overall and for subgroups of interest. Results for categorical variables are presented as absolute numbers and percentages. The distribution of continuous data was assessed with the Shapiro-Wilk test. Continuous variables were described as means (SD) if the dataset was normally distributed or as medians (interquartile ranges) if not.
To compare age and amount of excised tissue (size) in relation to the variables of interest, we used nonparametric tests, specifically, the Mann-Whitney U test for 2 datasets and the Kruskal-Wallis test for 3 or more datasets. To compare categorical variables we used the Pearson χ2 test. The level of significance was set at P<.05.
To evaluate whether the surgeon's specialty was independent of other known variables (patient age and tumor location, size, and histologic subtype), we used multivariable logistic regression analysis with backward stepwise selection of variables (significance level, P<.05).
All calculations were performed with SPSS software, version 18. Each subanalysis was performed only on tumors for which the relevant information was on record.
ResultsA total of 750 patients underwent surgery to remove 921 BCCs (mean of 1.23 tumors per patient). Most of the patients (621 [82.8%]) had a single tumor, 100 (13.3%) had 2 tumors, and 29 (3.8%) had more than 2 (maximum, 7 tumors). Slightly more patients were men (429 [57.2%]). The median age was 73 years, with no significant differences according to sex (men, 74 years; women, 73 years).
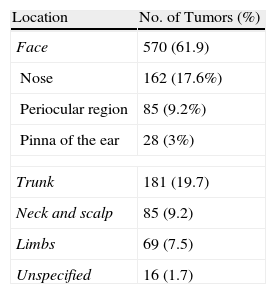
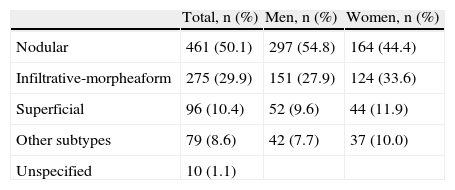
Tumor locations and histology are summarized in Tables 2 and 3, respectively. In both men and women, the most frequent location was the face, followed by the trunk. Median ages by tumor location were 70 years for patients with tumors on the trunk, 75 years for patients with tumors on the face or limbs, and 76 years for patients with neck and scalp tumors (P<.001). The median age was lower in the group of patients with superficial BCCs (70 years) than in the group with infiltrative-morpheaform tumors (76 years). Analyzing for frequency of histologic subtypes in different locations, we found that nodular BCCs were the most common in all locations. Infiltrative-morpheaform BCCs were the second most common type, except on the trunk, where superficial tumors ranked second in frequency. Nodular and infiltrative-morpheaform tumors were found mainly on the face, while superficial tumors were most often located on the trunk (P<.005).
Information on tumor size was available for only 368 BCCs. For cases in which this variable had been recorded, the median diameter at the widest part was 8.0mm. As tumor size had been recorded in fewer than half the tumors, we chose to analyze size of the block of excised tissue, information which was available for 919 excisions. The median diameter at the widest section of the excised tissue was 17.0mm. Larger blocks were excised from men (median diameter, 17.5mm) than from women (median diameter, 15.0mm) (P<.001). Analyzing size of excised tissue by location, we found that more tissue was removed when BCCs were on the limbs, trunk, neck, and scalp (median diameter, 20.0mm for all 3 locations) than when the tumor was on the face (median diameter, 15.0mm) (P<.001). Analyzing the relation between histologic subtype and median diameter of excised tissue, we found that larger amounts were removed when the BCC was an infiltrative-morpheaform tumor (median diameter, 20.0mm) than when it was a nodular BCC or other type (median diameter, 15mm) (P<.001).
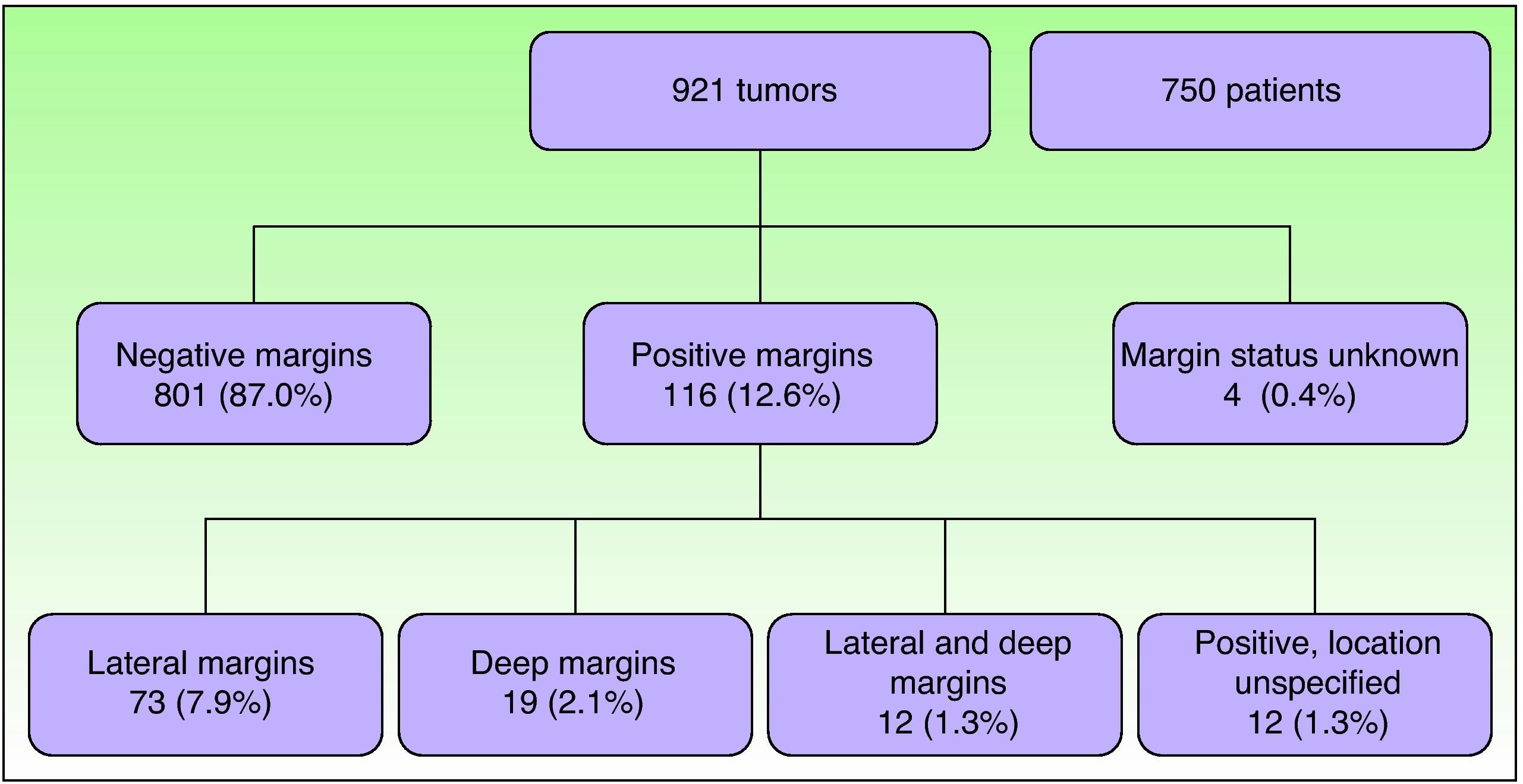
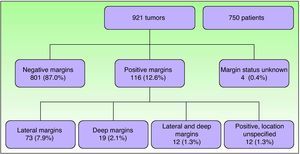
Assessment of Surgical Margins in the Series OverallOf the 921 tumors excised, the margins of 801 (87.0%) were tumor-free (negative). No information on margin status had been specified for 4 tumors. Of the 116 tumors with positive margins (12.6%), tumor cells were found in the lateral margins in the largest number of cases (73). Both deep and lateral margins were positive in only 12 tumors (Fig. 1). There were no significant differences between the positive-margin rates for men and women.
Analyzing by location, we saw the highest rate of incomplete excision in facial tumors (80.9%), followed by neck and scalp (7.8%), trunk (7.0%), and limb tumours (4.3%). The positive-margin rates were 16.4% for the face, 10.6% for the neck and scalp, 7.2% for the limbs, and 4.4% for the trunk. Of the 275 BCCs in complicated locations (162 on the nose, 85 in the periocular region, and 28 on the pinna of the ear), 57 (21%) had positive margins (vs. 58 of the remaining 628 excisions [9.2%]).
The histologic subtype was recorded for 114 of the 116 tumors with positive margins. More than half of the 114 were infiltrative-morpheaform tumors (71 [62.3%]) and nearly a quarter were nodular tumors (27 [23.7%]). Infiltrative-morpheaform tumors were thus associated with the highest relative risk of margin positivity: the 71 tumors with positive margins represented 25.8% of all tumors of this subtype. Superficial tumors with positive margins (7) were associated with considerably less risk (7.3% of such tumors), as were positive-margin nodular tumors (7, accounting for 5.9% of this type). Tumors excised with negative margins were smaller (median diameter, 15mm) than those with positive margins (median diameter, 17mm) (P=.006).
Assessment of Margins by Surgeon's SpecialtyDermatologists excised 549 tumors (59.6%). Plastic surgeons excised the next largest number (198 tumors [21.5%]), followed by general surgeons (143 tumors [15.5%]). Only 30 tumors (3.3%) were excised by other specialists (ophthalmologists, maxillofacial surgeons, or ear-nose-throat specialists). In 1 case, the surgeon's specialty was not recorded. We analyzed results for dermatologists in comparison with all other specialists together.
No differences between specialties were observed in relation to patient sex. The median age was lower for dermatologists’ patients than for nondermatologists’ (73 vs. 75 years, P=.001). By individual specialties, the median patient ages were 73 years for dermatology and general surgery, 76 years for plastic surgery, and 77.5 years for other specialties. No differences in tumor location were found between dermatologists and nondermatologists. In both groups, the face was the most common location (accounting for 62.9% of tumors excised by dermatologists and 63.2% of those removed by others). As expected, nodular tumors were the ones most often removed by both surgeon groups, followed by infiltrative-morpheaform tumors. However, analyzing by individual specialties, we did observe some significant differences (P=.018) in the frequencies of histologic subtypes. Nodular tumors accounted for 54.4% (298/548) of the tumors excised by dermatologists and for 45.0% (163/362) of the excisions by other specialists. The prevalence rates of infiltrative-morpheaform tumors also differed: 35.4% (128/362) of tumors removed by nondermatologists and 26.8% (147/548) of those removed by dermatologists were of this subtype. The percentages of other subtypes were similar between specialties. The analysis of sizes showed that the median maximum diameter excised was 16mm for dermatologists and 17mm for nondermatologists (nonsignificant difference). Among the nondermatologists, plastic surgeons removed the largest amounts of tissue (median diameter, 20mm) and general surgeons the next largest (14mm). The median maximum diameter of the block of excised tissue was 10mm for the group of other specialists (P<.001).
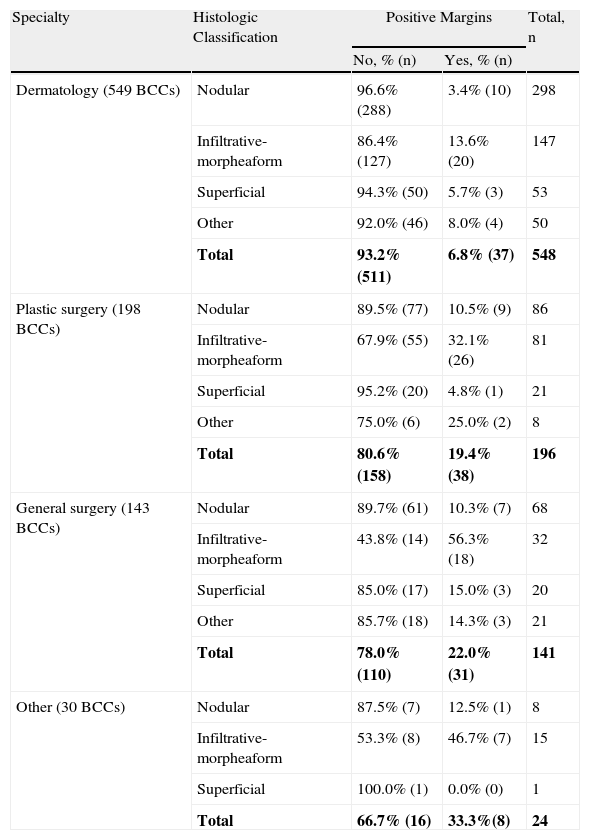
Positive margins were identified for 6.7% (37/549) of the tumors excised by dermatologists and 21.5% (79/367) of those removed by nondermatologists. Positive-margin rates by nondermatology specialties were 19.3% (38/197) for plastic surgeons, 22.4% (32/143) for general surgeons, and 33.3% (9/27) for other specialists (Table 4).
Margin Status, by Surgeon's Specialty and Tumor Histologic Classificationa
| Specialty | Histologic Classification | Positive Margins | Total, n | |
| No, % (n) | Yes, % (n) | |||
| Dermatology (549 BCCs) | Nodular | 96.6% (288) | 3.4% (10) | 298 |
| Infiltrative-morpheaform | 86.4% (127) | 13.6% (20) | 147 | |
| Superficial | 94.3% (50) | 5.7% (3) | 53 | |
| Other | 92.0% (46) | 8.0% (4) | 50 | |
| Total | 93.2% (511) | 6.8% (37) | 548 | |
| Plastic surgery (198 BCCs) | Nodular | 89.5% (77) | 10.5% (9) | 86 |
| Infiltrative-morpheaform | 67.9% (55) | 32.1% (26) | 81 | |
| Superficial | 95.2% (20) | 4.8% (1) | 21 | |
| Other | 75.0% (6) | 25.0% (2) | 8 | |
| Total | 80.6% (158) | 19.4% (38) | 196 | |
| General surgery (143 BCCs) | Nodular | 89.7% (61) | 10.3% (7) | 68 |
| Infiltrative-morpheaform | 43.8% (14) | 56.3% (18) | 32 | |
| Superficial | 85.0% (17) | 15.0% (3) | 20 | |
| Other | 85.7% (18) | 14.3% (3) | 21 | |
| Total | 78.0% (110) | 22.0% (31) | 141 | |
| Other (30 BCCs) | Nodular | 87.5% (7) | 12.5% (1) | 8 |
| Infiltrative-morpheaform | 53.3% (8) | 46.7% (7) | 15 | |
| Superficial | 100.0% (1) | 0.0% (0) | 1 | |
| Total | 66.7% (16) | 33.3%(8) | 24 | |
Abbreviation: BCC, basal cell carcinoma.
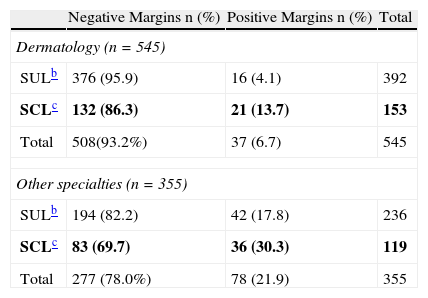
The results were similar for tumors at complicated sites. Dermatologists operated on 153 of these tumors and nondermatologists on 122. Margin status was unrecorded for 3 of the complicated tumors. Positive margins were observed in 13.7% (21/153) of the complicated tumors excised by dermatologists whereas that percentage was twice as high for nondermatologists, at 30.3% (36/119) (Table 5).
Margin Status, by Complicated vs. Uncomplicated Tumor Location and Surgeon's Specialtya
| Negative Margins n (%) | Positive Margins n (%) | Total | |
| Dermatology (n=545) | |||
| SULb | 376 (95.9) | 16 (4.1) | 392 |
| SCLc | 132 (86.3) | 21 (13.7) | 153 |
| Total | 508(93.2%) | 37 (6.7) | 545 |
| Other specialties (n=355) | |||
| SULb | 194 (82.2) | 42 (17.8) | 236 |
| SCLc | 83 (69.7) | 36 (30.3) | 119 |
| Total | 277 (78.0%) | 78 (21.9) | 355 |
Abbreviations: SCL, surgically complicated locations (nose, periocular region, and pinna of the ear); SUL, surgically uncomplicated locations (all remaining sites).
The higher prevalence of positive margins in excisions by nondermatologists cannot be attributed to patient age, BCC location, amount of excised tissue (diameter), or histologic classification. If the surgeon was not a dermatologist, the likelihood that margins would be positive was nearly 4-fold higher (odds ratio [OR], 3.8; 95% CI, 2.5–5.7). If the operator was a plastic surgeon, the likelihood of margin positivity was more than 3-fold higher than if the operator was a dermatologist (OR, 3.3; 95% CI, 2.0–5.4). The likelihood was about 4-fold higher if the operator was a general surgeon (OR, 3.9; 95% CI, 2.4–6.7). Finally, if the operator was a maxillofacial surgeon, ear-nose-throat specialist, or ophthalmologist (the 3 grouped as a single category), the likelihood of positive margins was nearly 7-fold higher (OR, 6.9; 95% CI, 2.9–16.4).
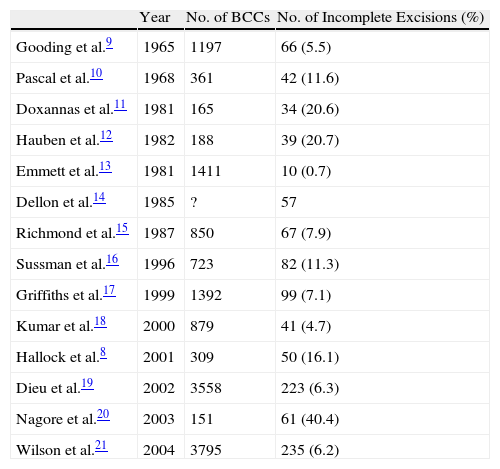
DiscussionMost BCCs are treated by surgical excision. Factors that influence the choice of one treatment over another include patient age, tumor location, histologic subtype, and tumor status as a primary or recurrent BCC.7 Treatment is usually curative, but in a non-negligible percentage of cases the tumor has invaded the surgical margins, which are then classified as positive. It is interesting that the prevalence of positive margin status is higher in retrospective studies than in prospective ones. Hallock and coworkers8 found that 15.7% of excised nonmelanoma skin cancers had positive margins in their series. In other series the prevalence of positive margin status after BCC excision has ranged from 6.5% to 20.7%.8Table 6 summarizes the prevalences of margin positivity after conventional excisions of BCCs in various published series.8–21
Summary of the Prevalences of Positive Margin Status in Other Studies of Basal Cell Carcinoma Excisions.
| Year | No. of BCCs | No. of Incomplete Excisions (%) | |
| Gooding et al.9 | 1965 | 1197 | 66 (5.5) |
| Pascal et al.10 | 1968 | 361 | 42 (11.6) |
| Doxannas et al.11 | 1981 | 165 | 34 (20.6) |
| Hauben et al.12 | 1982 | 188 | 39 (20.7) |
| Emmett et al.13 | 1981 | 1411 | 10 (0.7) |
| Dellon et al.14 | 1985 | ? | 57 |
| Richmond et al.15 | 1987 | 850 | 67 (7.9) |
| Sussman et al.16 | 1996 | 723 | 82 (11.3) |
| Griffiths et al.17 | 1999 | 1392 | 99 (7.1) |
| Kumar et al.18 | 2000 | 879 | 41 (4.7) |
| Hallock et al.8 | 2001 | 309 | 50 (16.1) |
| Dieu et al.19 | 2002 | 3558 | 223 (6.3) |
| Nagore et al.20 | 2003 | 151 | 61 (40.4) |
| Wilson et al.21 | 2004 | 3795 | 235 (6.2) |
Abbreviation: BCC, basal cell carcinoma.
When margins are negative we assume that excision is complete. Whether a finding of negative status is reliable or not depends on several factors, such as the number of histologic sections that have been extracted and examined, the size of the tumor, and the skill of the pathologist. However, it is estimated that only a small proportion of the entire surgical margin is examined in conventional histologic protocols.
This retrospective study determined the prevalence of positive margins of BCCs excised by operators from different surgical specialties. We believe that correct clinical examination and identification of tumor borders (which are often hard to distinguish) are of vital importance when planning a curative procedure in oncologic surgery.
Our study shows that the prevalence of positive margin status is lower when dermatologists excise these tumors (Table 4). The prevalence rate we observed for dermatologists’ excisions is among the lowest of those reported in the literature, and this finding is particularly interesting considering that ours was a retrospective study. In Spain, García-Solano and coworkers22 also reported lower positive-margin rates for dermatologists (7.7%) than for 2 other specialties (30.2% and 44.4%) in a series of 1104 excisions (including BCCs and squamous cell carcinomas). Another study of excisions performed by plastic surgeons reported a positive-margin rate of 8.4%.23 This figure is appreciably lower than the rates we have seen in Spain, but it is based on a prospective study in which a magnifying lens was used to determine tumor borders and in which the operators may have received a higher level of training in treating skin cancer.
The dermatologists in our series excised proportionally fewer infiltrative-morpheaform BCCs than nondermatologists did. Nonetheless, on analyzing margin clearance by specialty and histologic subtype, we still found that dermatologists had a lower rate of margin positivity even for these infiltrative-morpheaform tumors (13.6% for dermatologists, 32.1% for plastic surgeons, 56.3% for general surgeons, and 46.7% for others) (Table 2).
An interesting finding was the smaller amount of excised tissue in the group of tumors with positive margins, in which the median diameter was 15mm, as opposed to 17mm in the group of complete excisions (P=.006). This difference may have arisen as a result of operators’ attempts to take smaller margins to preserve as much normal peritumoral skin as possible, especially if we consider that 80.9% of the tumors with positive margins were taken from the face.
Statistical analysis showed that these between-group differences in the prevalence of positive margin status were unrelated to variables that might potentially make tumor excision difficult, such as a complicated location (face), more aggressive histologic subtype (infiltrative-morpheaform BCCs), larger size, or older patient age (associated with more concomitant diseases).
Dermatologists and nondermatologists treated patients of significantly different ages (median ages, 73 years and 75 years, respectively). However, we think these differences were clinically nonsignificant and may be attributable to the large size of the patient sample we studied.
The presence of residual tumor in margins does not always indicate that the tumor will regrow, and histologic classification and location are the best predictors of recurrence.2 BCC recurrence rates after incomplete excisions (those with positive margins) range from 0% to 44% (mean, 27%).2 Ríos-Buceta24 noted, when he looked at the records of 850 BCC excisions performed in his hospital, that the positive-margin rate was 6% (52 cases), but that, interestingly, the presence of residual tumor was demonstrated after reoperation in just 11 cases (21%). The approach to take when there are positive margins is hotly debated. Conservative management may be reasonable when margins are positive after BCC excision in some cases (for example, when the tumor was not in a high-risk location, when tumor classification indicates low aggressivity, when the positive margins are the lateral ones, and/or when the patient is of advanced age and has concomitant conditions). However, many cases call for further treatment, whether surgical or not (for example, adjuvant radiotherapy).
This study has several limitations. First, the retrospective collection of data meant that certain information, such as tumor diameter, was unavailable in many cases. Therefore, we analyzed the maximum diameter of the excised tissue as a surrogate for tumor size. These measurements, however, may be underestimated given that tissue contracts when stored in a formaldehyde solution. Another source of bias affects the total number of superficial BCCs, given that this type of tumor is often treated with cryotherapy, topical imiquimod, or other procedures. We also do not know if the excised tumors were primary or recurrent lesions. However, even though recurring lesions are surgically more complicated, we think that the lack of this information did not bias the results because in our practice setting the physician who first attends the patient is usually the one who also follows the case and performs later procedures. Finally, we had no information on whether the surgical approach was chosen on the basis of a clinical diagnosis or the analysis of a biopsy specimen. Knowledge of histologic classification can affect the surgeon's estimate of how much margin should be taken when removing a tumor, thus influencing whether the excision is complete or not.
Our study shows that positive-margin rates are lower in BCC excisions performed by surgeons in the dermatology department of Hospital Universitari Vall d’Hebron in comparison with operators who are plastic or general surgeons in the hospital. Factors such as patient age, tumor location and size or histologic subtype do not explain the higher positive-margin rates for nondermatologist surgeons. We believe that dermatologists’ greater ability to reach an accurate clinical diagnosis and skill in identifying tumor margins, which are often hard to discern, as well as their greater knowledge of the biologic behavior of BCCs may explain our findings. When excisions are incomplete, the second procedures that are often required increase health care expenditure and lengthen surgical wait lists. The dermatologist is the specialist who is best able to diagnose and treat skin cancer, as well as the one best equipped to lead multidisciplinary teams when tumors are particularly complicated to remove. Finally, we think it may be necessary to improve aspects of residency training in disciplines in which surgical procedures are performed on the skin.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We thank all members of the dermatology and pathology departments for their excellent routine performance of their work, which made this study possible.
We also thank Dr. Eva López Guerrero of the clinical pharmacology department for her invaluable help with the statistical analysis.
Please cite this article: Bassas P, et al. Evaluación de los márgenes quirúrgicos del carcinoma basocelular según la especialidad del cirujano. Actas Dermosifiliogr. 2013;104:133–40.