A 40-year-old man with no relevant past history came to our clinic for assessment of a subungual tumor affecting the fifth toe of the right foot that had first appeared approximately 2 years earlier. The lesion had initially grown rapidly and subsequently stabilized. The patient reported discomfort caused by friction against his footwear. There had been no episodes of bleeding or ulceration.
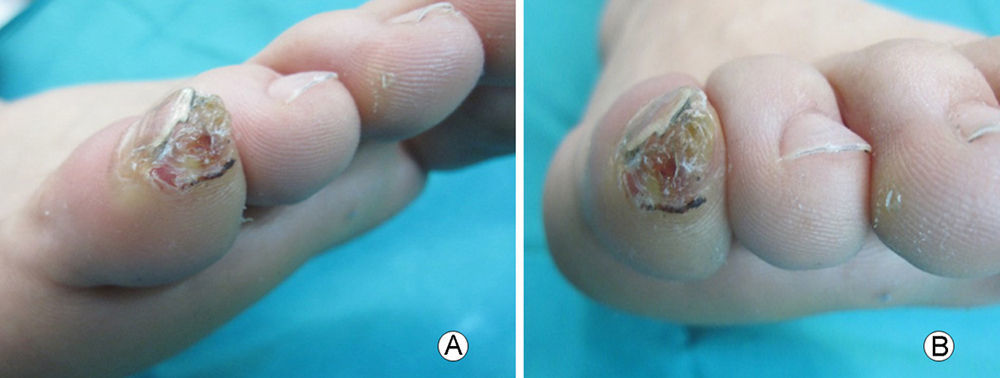
Physical ExaminationPhysical examination revealed a well-defined 1cm nodular subungueal lesion with a rough, hyperkeratotic surface that was causing the detachment of the nail (Fig. 1).
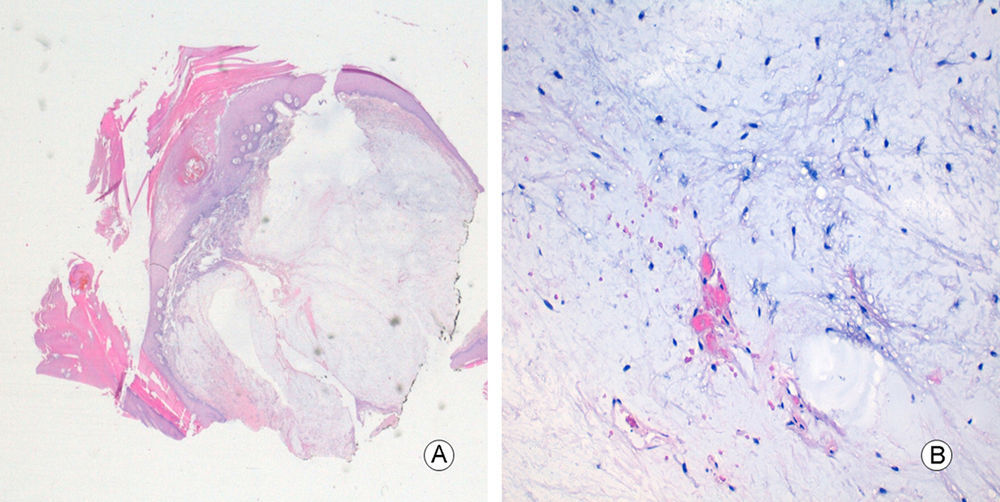
Additional TestsComplete excision of the lesion was performed. Histopathologic examination revealed a diffuse unencapsulated dermal lesion that extended to the deep margin of the resection specimen (Fig. 2A). The tumor contained a prominent myxoid stroma with low cellularity consisting of spindle-shaped cells, without atypia or mitotic figures. A vascular network of numerous elongated capillaries with narrow lumens was present. No inflammatory infiltrate was observed (Fig. 2B).
Immunohistochemistry was positive for CD34 only in the vascular component of the tumor and was negative for S-100 protein, epithelial membrane antigen, and MUC4 in the vascular component and the fibroblastic component.
What Is Your Diagnosis?
DiagnosisSubungual superficial angiomyxoma.
Clinical Course and TreatmentAfter excision of the subungueal tumor we performed a direct suture closure. Because the deep margin of the resected specimen was affected, we initially considered extending the surgical margins. However, the patient refused additional surgery and no evidence of tumor recurrence has been found during 12 months of follow-up.
CommentSuperficial angiomyxoma is a rare mesenchymal tumor classified as a benign cutaneous myxoma. It was first described by Carney et al.1 as being associated with Carney complex. It is mainly necessary to rule out Carney syndrome in patients with superficial angiomyxomas on the outer ear and patients with multiple lesions.2 We determined that our patient did not have Carney syndrome because the subungueal tumor was not accompanied by extracutaneous myxomas, skin pigmentation, or endocrine alterations.
Superficial angiomyxoma is more common in men, usually between 20 and 50 years of age. It normally appears as a single lesion3 and has a very heterogeneous clinical presentation. The lesion presents as a skin-colored papule, nodule, or polypoid lesion ranging from 1 to 5cm in size.2 The most common site in the reported series is the trunk, followed by the lower limbs and head or neck.4,5 It is very rare to find this lesion in a subungueal site, as in our patient. Only 3 cases of subungueal superficial angiomyxoma have been reported.6,7
Histologically, superficial angiomyxoma is a dermal tumor that extends into the subcutaneous tissue. The lesion usually presents a multi-lobed growth pattern with nodules of low cellularity immersed in a myxoid stroma.2,4,5 It contains cells of fibroblast morphology with fusiform, elongated, or stellate shapes that do not usually present atypia or mitotic figures. The presence of abundant vessels with narrow lumens is characteristic, and a perivascular neutrophilic and lymphocytic inflammatory infiltrate is seen in a third of cases. Immunohistochemical features of the lesions are fibroblast cells that are negative for CD34, smooth muscle actin, S-100 protein, epithelial membrane antigen, and desmin; however, myofibroblast differentiation may be present in some cases.2,3
For subungueal lesions,6,7 the main differential diagnosis is superficial acral fibromyxoma, a slow-growing benign tumor usually found on the toes and fingers.8 Histologically, this lesion presents as a well-defined dermal tumor that, in contrast to superficial angiomyxoma, has a less abundant myxoid stroma, higher cell density, increased microvascularization, and less prominent capillaries. Immunohistochemically, the lesion is characterized by CD34 expression in fibroblasts.8 In our patient, immunohistochemistry was negative for CD34 in the spindle-shaped fibroblastic component.
Superficial angiomyxoma is treated by surgery and local recurrences occur in 30% to 40% of cases.2,3,5 The lesion is considered to be a benign myxoid tumor. No metastatic cases have been reported to date.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Ayala D, Puglia V, Jordá E. Lesión tumoral hiperqueratósica subungueal. Actas Dermosifiliogr. 2017;108:361–362.