A 5-week-old girl with no relevant history apart from readmission at 6 days of life for hyperbilirubinemia requiring phototherapy (19.2mg/dL), at which time monocytosis (21.2%) was detected, was sent from the emergency department with progressive cutaneous lesions that had begun to appear a week earlier.
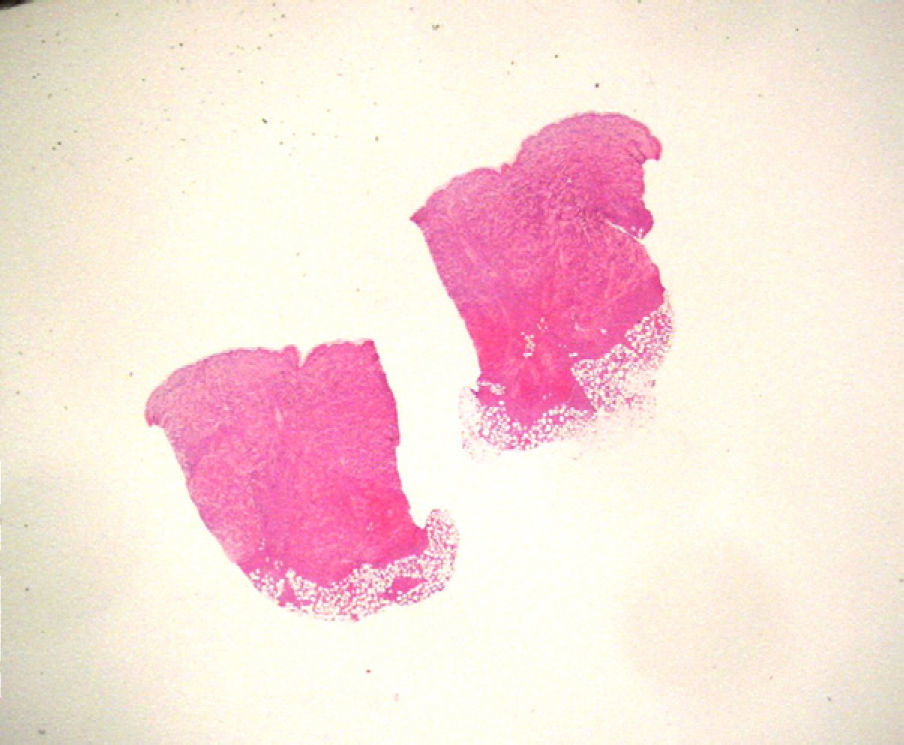
Physical ExaminationMultiple purpuric, erythematous papular and nodular lesions that felt infiltrated were distributed mainly on the torso, extremities, head, and perianal region; lesions were not found on the palms, soles, or mucosal surfaces (Fig. 1). Pallor and hepatosplenomegaly were also noted.
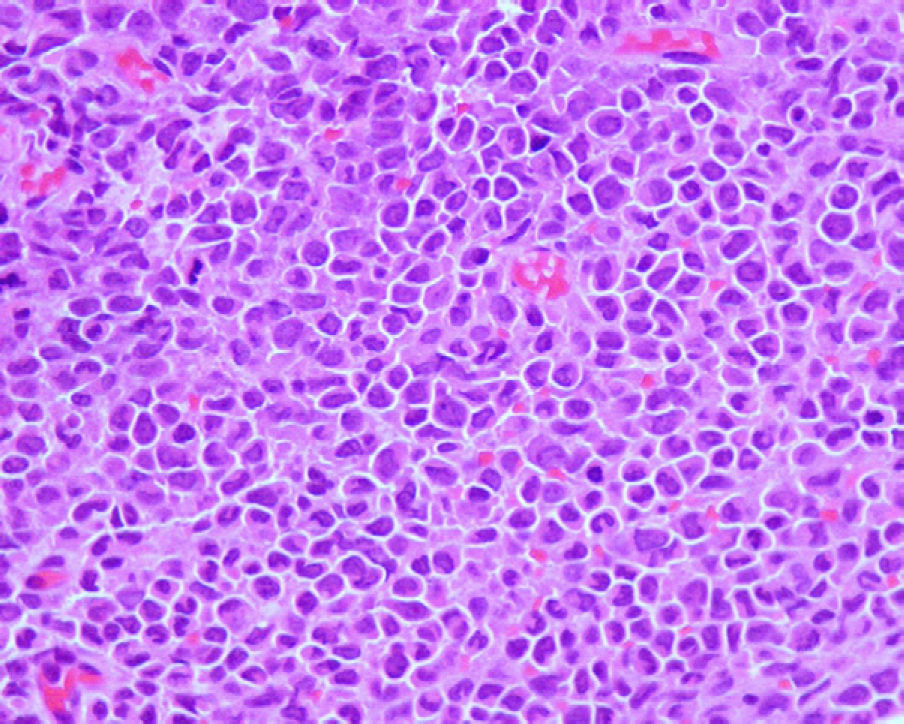
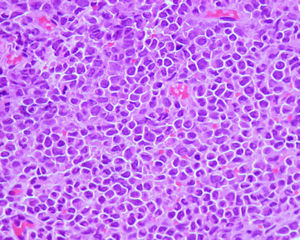
HistopathologyOn biopsy, an abdominal lesion showed a diffuse dermal infiltration, with involvement of subcutaneous tissue (Fig. 2); the infiltrate showed atypical cells with scant cytoplasm and a few mitotic figures (Fig. 3) that were positive for CD45, CD68, and CD4.
Additional TestsA new blood test revealed leukocytosis with monocytosis (70.2%); a blood smear showed 80% immature monocytes. Ultrasound identified hepatosplenomegaly and mild pulmonary stenosis. Serology was negative for TORCH infections (toxoplasmosis, other infections, including syphilis, parvovirus, and coxsackievirus, rubella, cytomegalovirus, herpes simplex virus).
What Is Your Diagnosis?
DiagnosisCongenital leukemia cutis.
Clinical Course and TreatmentAfter diagnosis, bone marrow studies confirmed the presence of acute monocytic leukemia (class M5). Polychemotherapy was initiated according to the SHOP-LANL-2001 protocol, followed by hematopoietic progenitor cell transplantation. The patient later died at the age of 7 months.
CommentLeukemia cutis, which occurs when leukemic cells infiltrate skin tissue, has been documented in 25% to 30% of patients with congenital leukemia.1–6 Leukemia is considered congenital when it appears in the first 4 to 6 weeks of life.1–3,5 Acute myeloid leukemia is the most common congenital type and the one that most often involves the skin.1–6
Most patients present generalized violaceous nodules, with oral lesions appearing in 1% of cases. Adult monocytic leukemia, in contrast, involves oral infiltration much more frequently.1
This condition has been referred to as blueberry muffin baby syndrome1–4,6 because the lesions resemble these muffins. Similar clinical manifestations may be seen in other serious conditions, such as congenital TORCH infections, hemolytic disease of the newborn (blood type incompatibility), hereditary spherocytosis, twin-to-twin transfusion syndrome, or other proliferative processes (histiocytosis, neuroblastoma metastasis, or rhabdomyosarcoma).1–6
Congenital leukemia cutis has been reported in Spain and internationally.1–6 The most extensive literature review, published in 1993, reported cutaneous involvement in 56 out of 175 cases of congenital leukemia.1 Approximately 15 new cases of congenital leukemia cutis have since been reported.2–6
Cutaneous manifestations may be present during the terminal phase, once the leukemia has started, or at the initial stage of the disease (10% of cases), with skin lesions occurring before tumor cell blasts are detected in peripheral blood and bone marrow.2
The treatment of choice is chemotherapy with hematopoietic progenitor cell transplantation. Isolated cases of spontaneous remission have been reported, all in the absence of progressive leukemia or 11q23 translocations6 and some involving relapse after a certain number of weeks or years2,6; withholding treatment is therefore controversial.2
The role of the dermatologist is essential in the identification and early diagnosis of these cutaneous lesions because underlying severe systemic conditions may be present. If congenital leukemia cutis is suspected, a biopsy of the lesions and complementary immunohistochemical assays will provide key diagnostic information.
Conflict of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Fernández-Morano T, et al. Pápulas y nódulos en un lactante. Actas Dermosifiliogr. 2011;102:733-734.