Of the various causes of salivary gland fistula, the most common include accidental trauma and postoperative complications. Salivary gland fistula is characterized by marked discomfort due to drainage of saliva through the fistula, a phenomenon that usually intensifies with chewing. Proteolytic enzymes present in saliva can impair healing, leading to a chronic condition that can be difficult to resolve.1
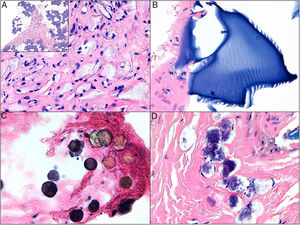
A 76-year-old woman presented with asymptomatic, multinodular, indurated subcutaneous plaques of 2.5×3 cm in diameter in both parotid regions that had appeared several months earlier (Fig. 1A). Injection of a filling material 12 years before was the only medical history of interest. The patient reported no symptoms prior to appearance of the plaques, which became evident following significant weight loss. Suspecting foreign body granuloma, a skin biopsy was obtained using a 4-mm punch. The biopsy showed infiltration of the parotid with 4 different filling materials: hyaluronic acid, polylactic acid, calcium hydroxyapatite, and a fourth unidentified material (Fig. 2).2
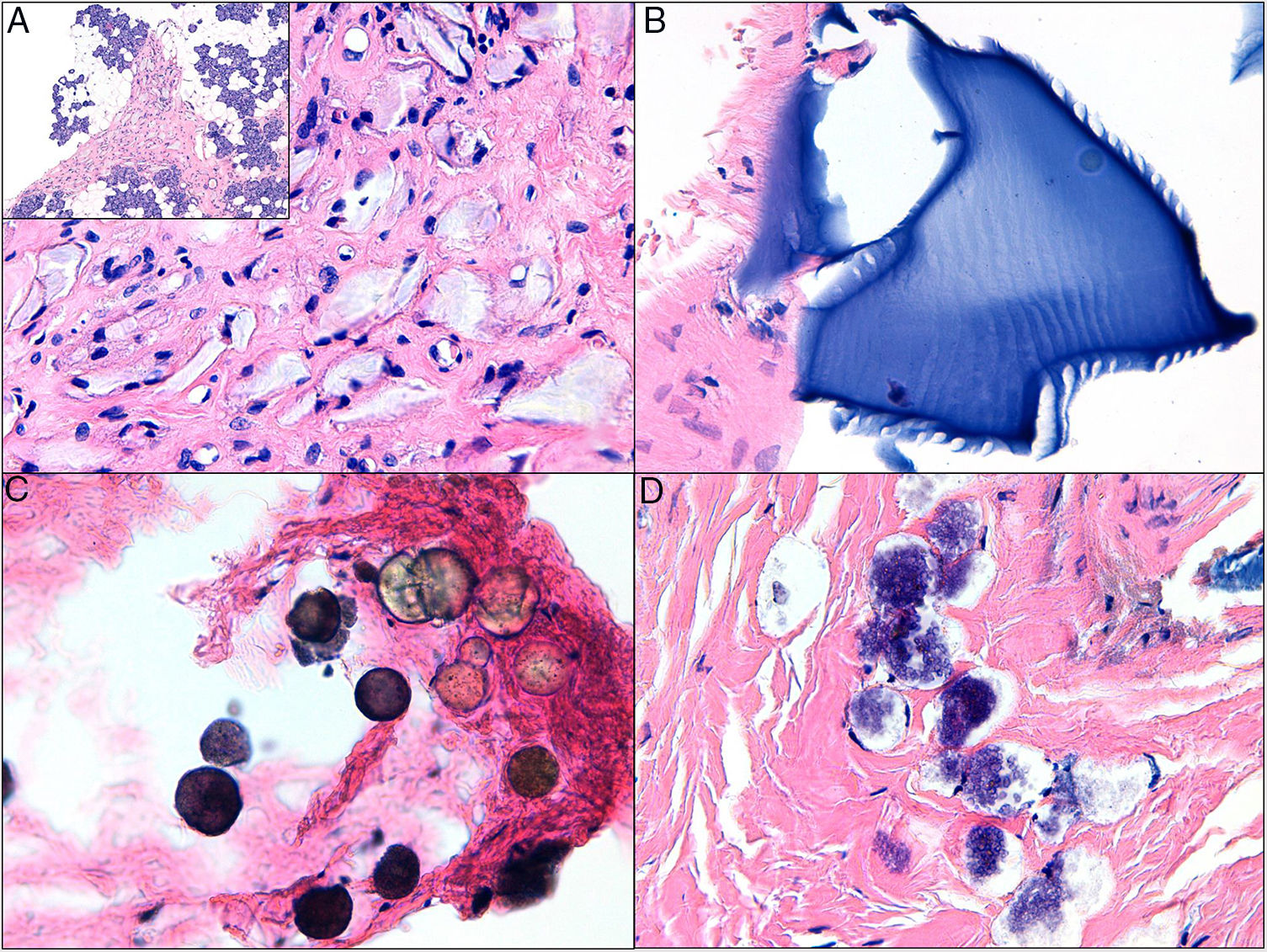
A, Indurated subcutaneous plaque of 2.5×3 cm in diameter in the parotid region. B, Parotid fistula with secretion of saliva from the defect 7 days after skin biopsy. C, Parotid fistula 3 weeks after treatment, before beginning botulinum toxin treatment. Botulinum toxin was injected subcutaneously at the 6 indicated sites around the defect. D, Final outcome after botulinum toxin treatment.
Skin biopsy composed mainly of parotid glandular tissue and 4 distinct synthetic materials (hematoxylin-eosin). A, Grayish fusiform material embedded in a hyaline stroma compatible with polylactic acid infiltration of the parotid glandular tissue. B, Polymorphous laminated basophilic material compatible with hyaluronic acid. C, Blackish-gray microspheres compatible with calcium hydroxyapatite. D, Unidentified basophilic foam-like material.
One week later the patient presented with secretion of saliva from the biopsy site, a phenomenon that clearly intensified with chewing. A reinforcing suture was placed in the wound and a compression bandage applied. No improvement in the patient's clinical signs was observed. Subsequent wound margin debridement and closure of the defect with interrupted sutures at the otorhinolaryngology department failed to achieve symptom control (Fig. 1B).
One week later the patient was seen for enlargement of the fistula. The margins were macerated and irritated, and the amount of saliva secreted had increased. We decided to locally administer botulinum toxin-A (Botox, Allergan Inc., Irvine, CA, USA); 100 U was diluted in 2 mL of physiological saline and 24 U of the solution was injected subcutaneously at 6 sites around the defect (Fig. 1C). While a clear decrease in the size of the defect was observed 2 weeks later the patient's symptoms persisted, and she received a second round of subcutaneous botulinum toxin-A injections (24 U). Four weeks later total closure of the fistula was achieved, with no treatment-related complications observed (Fig. 1D).
Parotid fistula most commonly occurs as a complication of parotid surgery, with incidences as high as 14% reported in some series. Fistulas can be classified according to duration: early fistulas last less than 6 weeks, while permanent fistulas last longer.3 This distinction is important. While both forms pose therapeutic challenges, the former tend to respond to conservative treatment with a compression bandage, whereas permanent fistulas tend to respond poorly and often require surgical intervention.
Injection of botulinum toxin-A is one form of treatment that has shown good results in recent years.4,5 The toxin temporarily blocks the release of parasympathetic cholinergic neurotransmitters, thereby reducing secretion by the salivary gland and facilitating closure of the fistula. Although the effect is temporary, this approach is minimally invasive, is associated with few complications, and is well tolerated.
Doses of botulinum toxin usually range from 10 U to 40 U, administered 2 to 4 weeks apart.6,7 A reduction in saliva secretion is observed after a few days. However, it is important to remind the patient that the maximum effect may not be observed for several weeks. While our patient underwent 2 rounds of botulinum toxin injections, it is highly likely that fistula closure could have been achieved with a single round of treatment.
Sialorrhea is treated with doses of 22.5 U per salivary gland, usually administered following ultrasound-guided blockade of the main endings of the facial nerve.5 In our patient, botulinum toxin was injected at several sites surrounding the defect in order to decrease the secretion of saliva in the area without completely blocking salivation.
The appearance of parotid fistulas as a complication after removal of skin tumors and foreign body granulomas near the parotid gland has been anecdotally described, and should be kept in mind when performing any invasive procedure in this region.6,8 In these cases, imaging techniques such as ultrasound, computerized axial tomography, and nuclear magnetic resonance imaging may be useful to attempt to identify the filling material used.9,10 Fine-needle aspiration, with or without ultrasound guidance, can also be used to obtain biopsies from sites of risk.
We have reported this case to highlight the risks associated with skin biopsy near the parotid gland and the excellent results that can be achieved with conservative treatment with botulinum toxin in parotid fistula patients.
The authors thank Dr. Víctor Traves, pathologist at the Instituto Valenciano de Oncología, Valencia, Spain.
Please cite this article as: Bancalari B. Fístula parotídea tras biopsia cutánea: tratamiento con toxina botulínica. Actas Dermosifiliogr. 2019;110:693–695.