Martorell hypertensive ischemic leg ulcer (HYTILU) is an ischemic lesion caused by the obstruction of small arterioles, in the absence of signs of vasculitis; it is frequently refractive and is extremely painful. Clinical presentation is characterized by rapid growth and difficult pain management.1,2 While there is no benchmark treatment for this lesion, it is essential to manage the inflammation and pain. The most common form of management, with dressing in a moist environment, provides unsatisfactory results. Treatment with punch grafting,3 however, is associated with greater anti-inflammatory and analgesic capacity, and shorter healing time.2,4,5
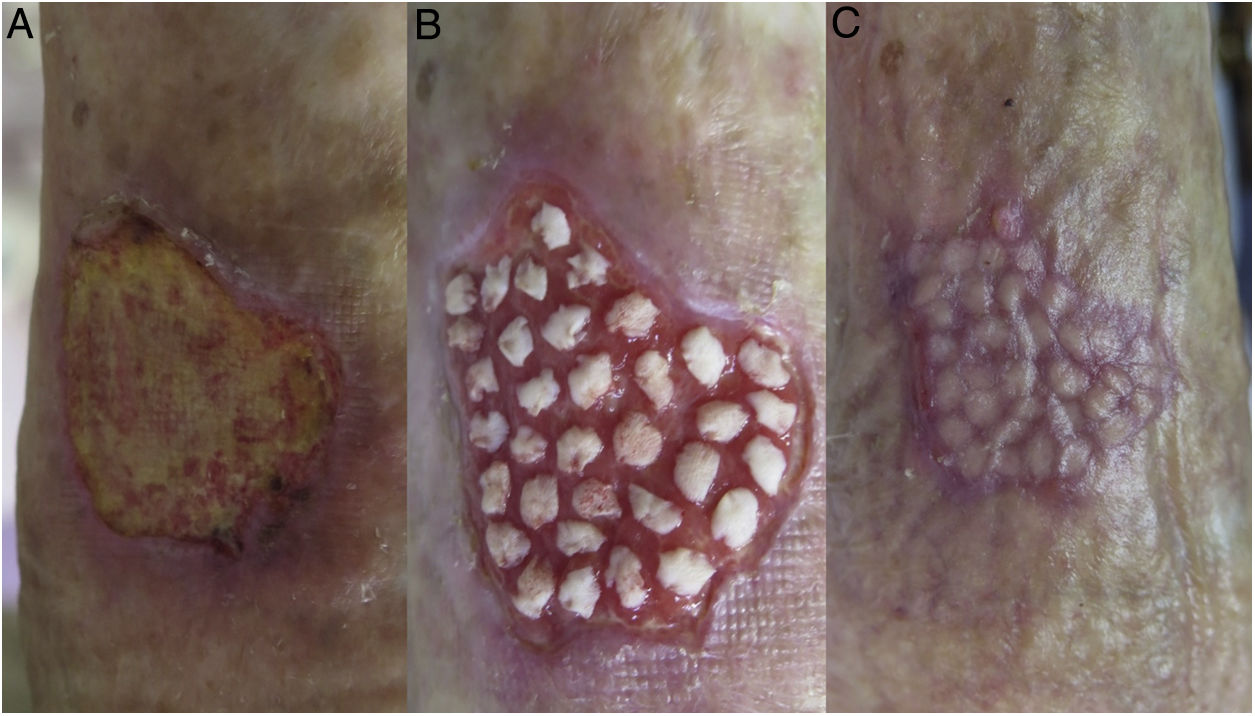
We report 3 clinical cases of Martorell HYTILU treated with punch grafting, with effective pain management and complete healing in 3 to 8 weeks. The patients were aged between 72 and 83 years and all of them had a history of hypertension and dyslipidemia. One of the patients had diabetes mellitus. They presented ulcers with similar clinical characteristics, with an erythematous-violaceous lesion that was painful to the touch, with irregular hyperemic borders, slough in the wound bed with lacunar infarcts, no clinical data suggesting infection, and a context of phlebolymphedema (Fig. 1A). The lesions were located on the distal and medial third of the anterior, lateral, and posterior surface of the lower extremities, and had developed over periods ranging from 2 months to 3 years; all the lesions were associated with traumatic triggering events. In the initial clinical assessment, the mean pain score on a visual analog scale (VAS) was 10/10, with pain occurring predominantly at night, and with no improvement after analgesic treatment, even with opioids, or after elevating the affected extremity. The distal pulses were present and the ankle-brachial pressure index (ABPI) was approximately 1 (normal range) in all the patients. Blood and urine workup revealed no significant findings. Blood pressure and glucose were normal during the healing process in all patients.
Initial treatment was with betamethasone 0.5% cream on the borders every 72hours for 15 days, autolytic debridement with twice-weekly dressing in a moist environment, and low-elasticity compression bandages (minimum estimated pressure, 20mmHg). This management provided adequate preparation of the bed in a period of between 2 and 3 weeks, with reduction of pain on the VAS of between 2 and 3 points. After adequate granulation tissue was obtained in the wound bed, fine punch grafting was performed (Fig. 1B). The patient was instructed to rest the limb during the first 5 days after the grafting procedure and wound care involved changing the dressing once per week (bioactive protease-inhibiting dressing with a polyester mesh and alginate as a secondary dressing), combined with compression bandages; the graft take rate was between 90% and 100%. Full epithelization was achieved between 3 and 8 weeks after grafting (Fig. 1C). No complications were recorded at the donor site (anterior lateral surface of the thigh) or at the recipient site.
Diagnosis of Martorell HYTILU is essentially clinical, although it has its own characteristic histology, which will reveal obstruction of the subcutaneous arterioles. The etiology and pathogenesis of the lesion are still not fully understood, although some studies associate the lesion with a history of long-term hypertension; however, hypertension, whether properly managed or not, is not considered sufficient and must therefore be associated with other abnormalities. The lesion is frequently associated with underlying diseases such as diabetes, obesity, chronic venous insufficiency, and peripheral artery disease. The most common local management option is dressing in a moist environment with bioactive bandages, despite the fact that this does not control the inflammatory process in Martorell HYTILU.1,2 Different authors have reported the analgesic effect of fine punch grafting in Martorell HYTILU.2,4 These split-thickness “postage-stamp” grafts, obtained using a punch, curette, or scalpel, include the epidermis and dermis, down to the superficial papillary dermis.5 In wounds with a considerable amount of slough, although the graft does not take adequately, vasodilating cytokines, growth factors and angiogenic factors are still released, which allows for modulation in arteriolar vasospasm.6 The analgesic effect of punch grafting, without prior administration of analgesics, has been reported 5hours after the grafting procedure, with regression of the erythematous-violaceous halo between 3 and 17 days after the graft.4,5
Adjuvant negative-pressure therapy is an interesting therapeutic option for promoting punch graft take, mainly in suboptimal beds and beds in complicated anatomical locations, such as the Achilles tendon.7
In our 3 cases of Martorell HYTILU, punch grafting allowed for healing periods of less than 2 months, with control of the associated pain. It is a safe and efficient therapeutic option that is easy to apply in the outpatient setting, with low additional morbidity for the patient.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Guisado Muñoz S. Tratamiento de la úlcera isquémica hipertensiva de Martorell con microinjertos autólogos en sello. Actas Dermosifiliogr. 2019;110:689–690.