Treatment of nail psoriasis remains a challenging and often disappointing situation.
ObjectiveTo compare the efficacy, adverse reactions and tolerability of treatment of nail psoriasis with PDL vs. Nd:YAG, in association with betametasona calcipotriol gel.
MethodsAn open, prospective intrapatient left-to-right study was designed. The right hand of each patient received treatment with PDL and the left hand with Nd:YAG. Betamethasone calcipotriol gel was applied once a day during the first week after each laser session. A total of four sessions were administered.
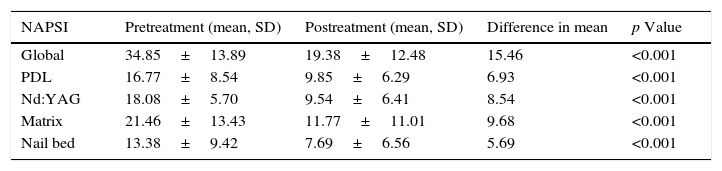
ResultsThe clinical efficacy was evaluated according to the NAPSI score.
All patients showed improvement in nail bed and nail matrix psoriasis. The global NAPSI mean declined in 15.46 (p<0.000). There was neither statistical difference between the reduction in nail bed and matrix NAPSI nor in the treatment with PDL vs. Nd:YAG. The administration of Nd:YAG was more painful. No serious adverse effects were documented.
LimitationsNo random assignment and the small number of patients.
ConclusionsPDL and Nd:YAG have proven to be an effective treatment for nail psoriasis with no serious adverse effect. No statistically significant difference was found between the two treatments.
El tratamiento de la psoriasis ungueal es una situación de difícil manejo y a menudo decepcionante para el dermatólogo.
ObjetivoComparar la eficacia, las reacciones adversas y la tolerabilidad del tratamiento de la psoriasis ungueal con PDL vs. Nd: YAG en asociación con gel de betametasona calcipotriol.
MétodosEstudio prospectivo abierto con control intrapaciente izquierda-derecha. La mano derecha de cada paciente recibió tratamiento con PDL y la mano izquierda con Nd: YAG. Se aplicó gel de betametasona calcipotriol una vez al día durante la primera semana después de cada sesión de láser en las 2 manos. Se administraron un total de 4 sesiones.
ResultadosLa eficacia clínica se evaluó de acuerdo con la escala NAPSI. Todos los pacientes mostraron una mejoría en las lesiones del lecho y de la matriz ungueal. La media global del NAPSI disminuyó en 15,46 (p<0,000). No hubo diferencia significativa entre la mejoría de las lesiones del lecho y la matriz ni en el tratamiento con el PDL vs. Nd: YAG. La administración de Nd: YAG fue más dolorosa. No se documentaron efectos adversos graves.
LimitacionesFalta de asignación aleatoria y muestra pequeña.
ConclusionesPDL y Nd: YAG han demostrado ser tratamientos eficaces para la psoriasis ungueal sin documentarse efectos adversos graves. No se encontró diferencia estadística significativa entre los 2 tratamientos.
Even though cutaneous signs and symptoms are the most common clinical manifestations of psoriasis, the nails can be involved in up to 78% of patients, reaching 95% if psoriatic arthritis is present.1 The longer the psoriatic lesions exist, the higher the frequency of nail changes will be. Furthermore, in a study involving 1728 patients with nail psoriasis 93.3% indicated that nail changes were cosmetically disturbing, 58.9%, reported restriction in their daily activities, and 51.8% referred pain.1
The clinical presentation has a wide spectrum of changes depending on the location of the pathology. Pitting, leukonychia, red spots in the lunula, nail plate crumbling, Beau lines, and trachyonychia are signs of nail matrix involvement. On the other hand, onycholysis, oil drop discoloration (salmon patch), subungual hyperkeratosis, and splinter hemorrhage indicate nail bed involvement.2,3 This differentiation is convenient because nail matrix psoriasis is expected to be more resistant to different therapeutic approaches.
Traditional therapies have focused on the inhibition of epidermal proliferation, inflammation, or both. However, it has recently been pointed out that the earliest changes noted in a new psoriatic lesion arise in the superficial dermal microvasculature4 and that these are necessary for maintaining clinical lesions. Because the psoriatic blood vessels play such an important role, acting on the abnormal psoriatic vasculature may be beneficial in psoriasis.
Material and methodsWe conducted a prospective intra-patient left-to-right controlled study. Patients with bilateral fingernail psoriasis were enrolled. The patients could have undergone prior topical or systemic treatment or be naive. Exclusion criteria were onychomycosis, concomitant treatment with drugs affecting the nail, use of permanent manicures, subungual hematoma, subungual nevus and history of trauma.
Signed consent forms were obtained from each patient before entering the study.
The initial evaluation included a complete medical history, physical examination, Nail Psoriasis Severity Index (NAPSI) score, and digital photographs. During every visit the NAPSI score and the digital photographs were updated and the patients were asked to identify their nail improvement and evaluate pain in both hands on a visual analog scale from 0 to 10 (patient global assessment: 0: no change; no pain, 10: total clearance, extremely painful). At the end of the sessions, the patient's satisfaction was evaluated with a visual analog scale, (0: not satisfy at all, not effective 10: very satisfy, very effective).
The right hand of each patient received treatment with Pulse Dye Laser (PDL) with a pulse duration of 0.4ms, an energy of 6J/cm2 and a beam diameter of 7mm, Whereas the left hand was treated with Nd:YAG with a beam diameter of 5mm, pulse duration of 35ms and an energy of 40J/cm2. All the nail plates, including the lunula, were treated with contiguous layers of spots with a 30% overlapping. The patient was instructed to apply betamethasone calcipotriol gel every 24h for a week in both sides.
A premedication involving paracetamol was given one hour before the session if requested by the patient. Treatment sessions were repeated every month for a total of four sessions.
ResultsThirteen patients (seven women, six men) were enrolled in the study. Two patients left the study at session 2 and 3 respectively, none of them due to adverse reactions. The mean age was 48±15 years and the majority had occupations that required regular use of the hands. Twenty three per cent of the patients (3 patients) had exclusive nail involvement, 31% (4 patients) associated psoriatic arthritis and 38% have not received previous treatment. None of those that have been treated before with topical (corticosteroids, calcipotriol, retinoids, or a combination of these) or systemic therapy (acitretin, methotrexate) have showed previous improvement of their nail involvement.
Clinical efficacy was evaluated statistically according to global NAPSI score, nail bed NAPSI score (onycholysis, nail bed hyperkeratosis, oil drop discoloration, splinter, hemorrhage) and nail matrix NAPSI score (pitting, leukonychia, red spots in lunula, nail plate crumbling).
All patients experience improvement in the global, matrix and nail bed NAPSI score (Figs. 1–4). The pre-treatment global NAPSI mean was 34.85±13.898 and the post-treatment was 19.38±12.48 with a diminution of the global mean of 15.46 (p<0.000) (Table 1). Unlike other studies, we did not find a significant difference between the drop in the matrix and the nail bed NAPSI score mean.
Comparison of the NAPSI score before and after the treatment of nail psoriasis with PDL (right hand) and Nd:YAG (left hand).
| NAPSI | Pretreatment (mean, SD) | Postreatment (mean, SD) | Difference in mean | p Value |
|---|---|---|---|---|
| Global | 34.85±13.89 | 19.38±12.48 | 15.46 | <0.001 |
| PDL | 16.77±8.54 | 9.85±6.29 | 6.93 | <0.001 |
| Nd:YAG | 18.08±5.70 | 9.54±6.41 | 8.54 | <0.001 |
| Matrix | 21.46±13.43 | 11.77±11.01 | 9.68 | <0.001 |
| Nail bed | 13.38±9.42 | 7.69±6.56 | 5.69 | <0.001 |
The left hand treated with Nd:YAG diminished in 8.54 points versus the right hand with PDL 6.93 with no statistical significant difference. The visual analog scale ranging from 0 to 10 to evaluated the pain demonstrated that the treatment with Nd:YAG was more painful than the PDL with a mean of 5.4±3.3 compared to 2.9±1.8. The 84% of the patients showed an improvement in the symptomatology. Compared to other therapies, the visual analog scale, which evaluated patient's satisfaction with laser treatment showed a high preference for the former with a mean of 8.4±1.2 for the laser treatment compared to 1.5±0.5 of other therapeutics approaches Only transient petechiae were documented. No other adverse effects were observed.
DiscussionLaser therapy has proved to be a safe and effective therapy for nail plate psoriasis. Our study suggests that it use, alone or in combination with other therapeutic modalities, can help to improve this resistant form of psoriasis.
Many studies have already shown the efficacy of PDL in the treatment of plaque type psoriasis, which exhibits the characteristics of angiogenesis and increased vascularity. Besides destruction of blood vessels, PDL can reduce the number of helper T cells in the dermis, eliminate the extravasation of inflammatory mediators into the interstitium and normalize epidermal proliferation, which improves the clinical signs of psoriasis vulgaris.2,4
In 2009, Fernandez-Guarino et al. studied the efficacy of PDL in nail psoriasis treatment, revealing excellent results, with 33% improvement after 12 weeks of treatment and 58% improvement after 24 weeks of treatment.2
In some studies the clinical improvement was more prominent in the nail bed lesions, particularly onycholysis and subungual hyperkeratosis.5 In our study, however this difference was not statistically significant. This could possibly be justified because this improvement will appear later as the nail plate grows, so a follow up over several months is necessary to perceive these changes.
To our knowledge there are not studies that have either evaluated the efficacy of Nd:YAG for the treatment of nail psoriasis or compared its efficacy to PDL.
One could see how treatment of deeper vessels in psoriatic lesions could improve the results of laser therapy. This could be achieved by using Nd:YAG which has the ability to penetrate deeper into the dermis. We find a slight difference that privileges Nd:YAG but the results were not statistically significant. Besides, the treatment with Nd:YAG was more painful, therefore its use does not appear to be justified if the PDL is available.
Due to the fact that the optimum parameters for PDL and Nd:YAG for treatment of psoriasis and nail psoriasis, have not been clarified, parameters in our study were, to some extent, compatible with the parameters of previous studies.2,4–6
It is known that the combination of laser and topical treatment can enhance the positive results of the therapy.4 Therefore, we used a coadjuvant treatment with betamethasone calcipotriol gel to improve the outcome. Patients who were neither naïve or have not responded to previous or concurrent topical or systemic therapy were enrolled. We found improvement in both groups, even in those who were refractory to systemic therapy. These results suggest the benefits of this therapy alone, especially for those patients who have an exclusive nail involvement or as a coadjutant treatment to other therapeutic modalities for those with more widespread disease.
Patient's satisfaction was higher than that demonstrated with other therapeutical modalities. The resolution of the symtomatology was documented in the majority of the participants. No differences in this matter were observed when the two types of laser were compared. No serious adverse effects were notice. A long follow up is necessary in order to decide whether further sessions of laser are needed to maintain the response for a long period of time.
The main limitation of this study is the low sample size, not previously calculated.
In conclusion, laser therapy has showed to be effective and safe for nail plate psoriasis with high patient's satisfaction. It could be used alone or combined with different therapeutic modalities, being especially beneficial with topical treatments. Nd:YAG did not seem to add any benefit to the use of PDL. Even though clinical trials are needed to establish a protocol, the present study can guide clinicians to introduce this therapy for all kinds of nail psoriasis.
Ethical responsibilitiesProtection of people and animalsThe authors state that the procedures conformed to the ethical standards of human experimentation committee responsible and according to the World Medical Association and the Declaration of Helsinki.
Confidentiality of dataThe authors declare that this article does not appear patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of patients and/or subjects referred to in Article consent. This document is held by the corresponding author.
Conflict of interestMónica Roncero has received funding for attendance to the AEDV Conference in 2014 following the completion of the study.