Tuberous sclerosis complex (TSC), an autosomal dominant disorder with variable expressivity, is caused by mutations in the tumor suppressor genes TSC1 and TSC2, which encode hamartin and tuberin proteins, respectively.1–3 TSC manifests with the formation of hamartomas in multiple organs, mainly the skin, central nervous system, kidneys, lungs, and heart.1–3 Vascular anomalies associated with overgrowth, hypertrophy, or gigantism are uncommon in TSC.2 We report the case of a TSC patient with congenital hypertrophy and combined vascular malformations of the left arm.
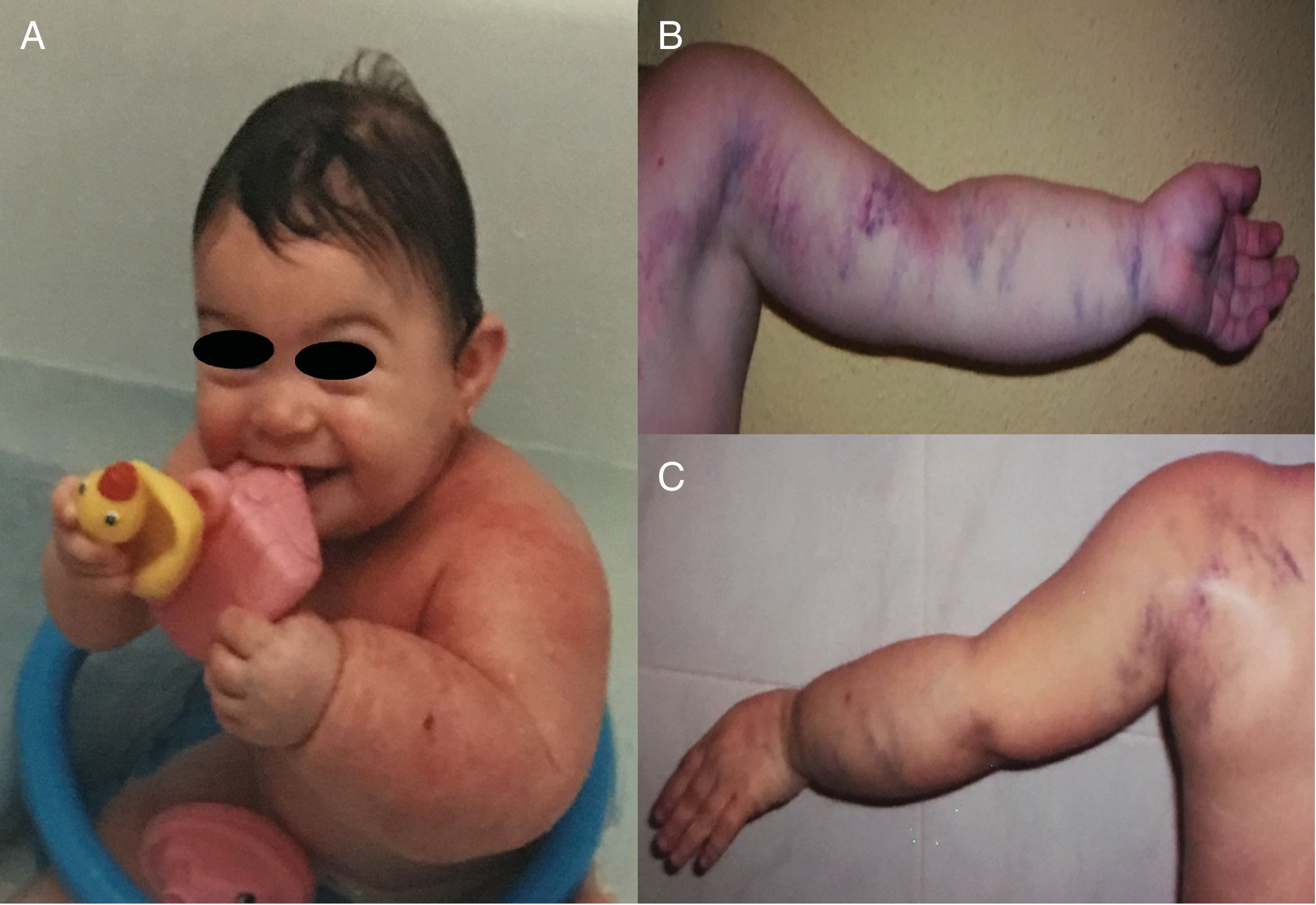
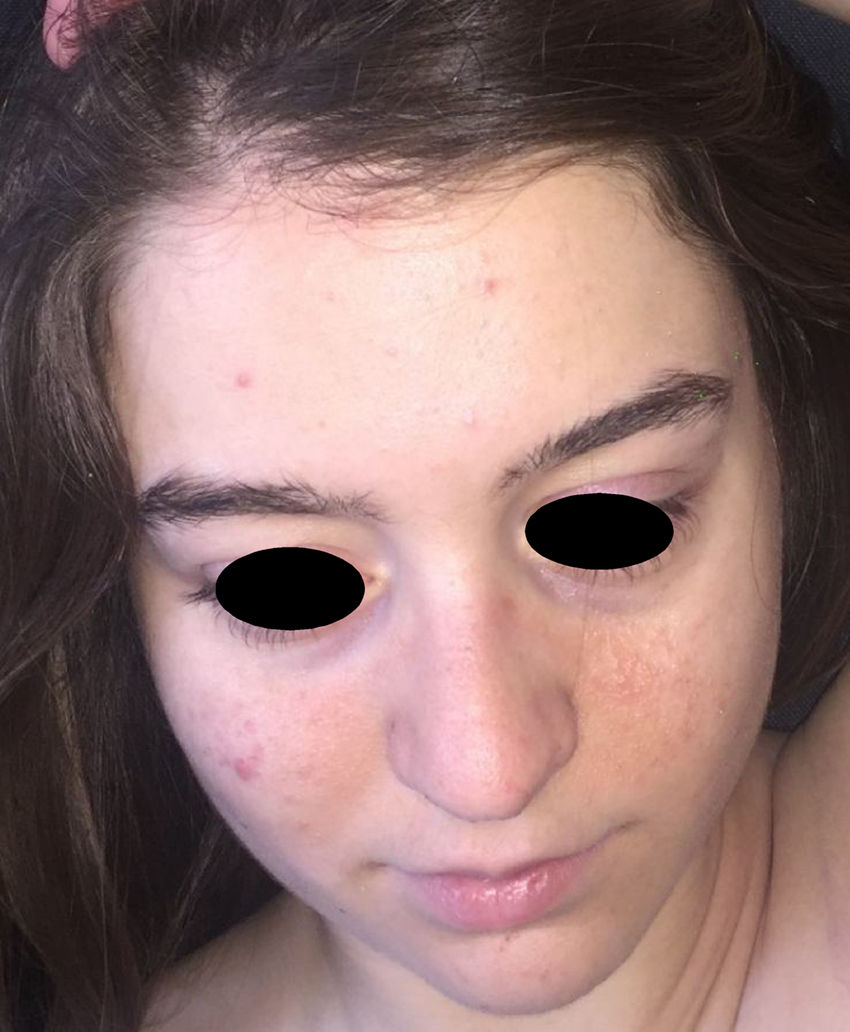
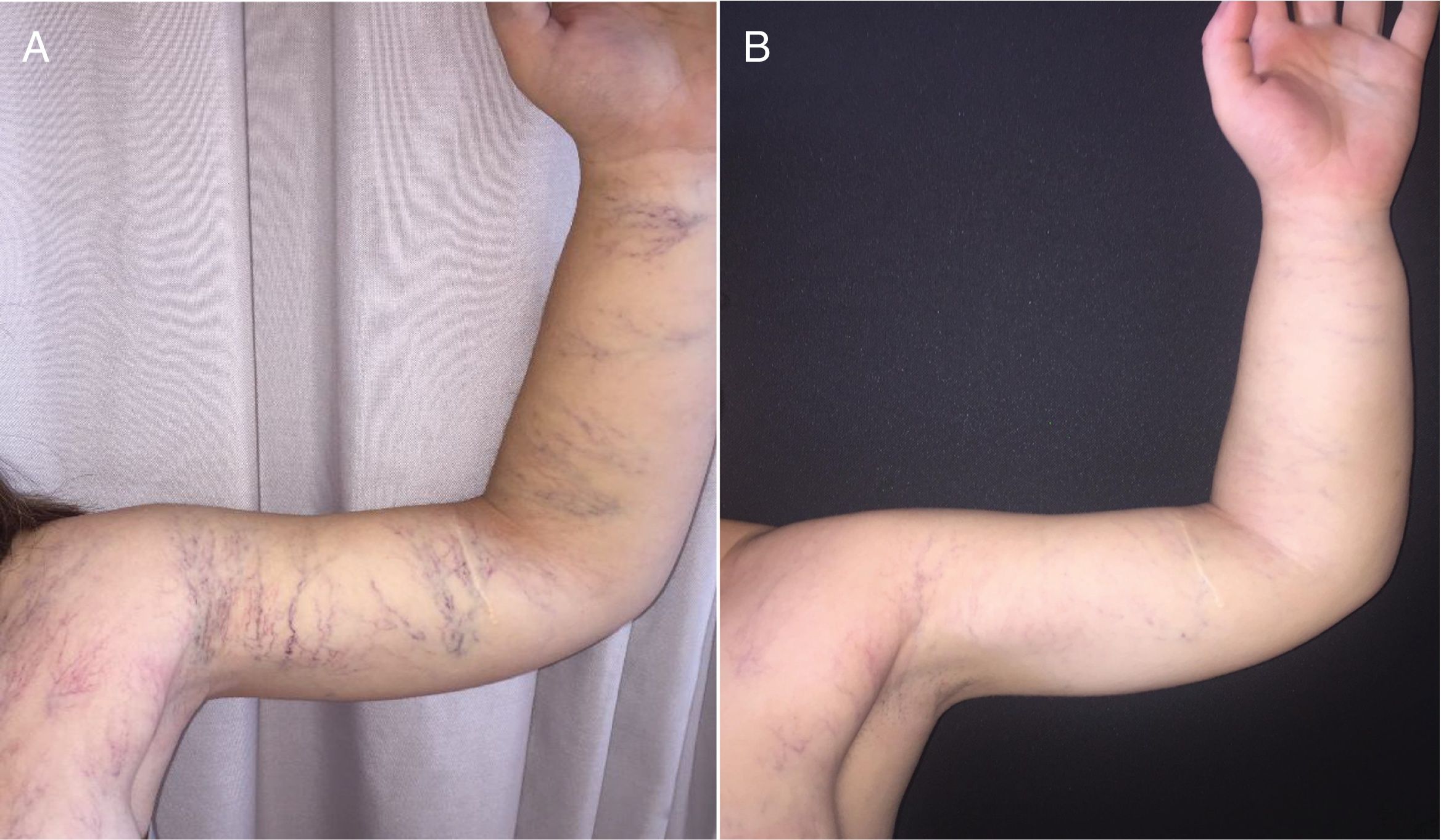
A 17-year-old adolescent girl, who was diagnosed with TSC at 9 years of age, was followed from birth for hypertrophy and combined vascular malformations of the left arm. The diagnosis of TSC was confirmed upon identification of the c.235G>T mutation in TSC2 in heterozygosis, in the absence of any clinical signs of the disease. The patient's mother carried the same mutation and presented clinical signs of TSC. A physical examination carried out during the first months of life revealed telangiectatic and purpuric vascular lesions (Fig. 1A) accompanied by multiple visible capillaries and venous vessels (Fig. 1B and C) on the left arm, the diameter of which was enlarged. No skin lesions indicative of TSC were observed. Doppler ultrasound performed at 20 days of age revealed no alterations of the arterial or deep venous systems. At 4 months of age, a deep skin biopsy, which included muscle, showed enlargement of the blood vessels in the dermis and subcutaneous tissue suggestive of capillary and venous malformations, in addition to ectasia of the lymphatic vessels. Immunohistochemistry revealed positive staining for D2-40 and negative staining for GLUT1 and WT1. No alterations in muscle tissue were observed, and atypia and mitotic figures were absent. Hypopigmented macules on the thighs, facial angiofibromas (Fig. 2), and periungual fibromas on the hands and feet became more evident once the patient reached 8 years of age, and were accompanied by Shagreen patches on the trunk that were compatible with TSC, which was confirmed by genetic study. A general physical examination and imaging techniques including conventional radiology, abdominal and pelvic ultrasound, brain magnetic resonance imaging, and cardiac ultrasound revealed no systemic alterations. The patient was diagnosed with predominantly lymphatic combined vascular malformation associated with TSC caused by TSC2 mutation. At age 11 years the patient began treatment with oral rapamycin (0.8 mg/m2/12 h) for 6 months. Because no decrease in the circumference of the affected arm was observed and the patient showed no systemic signs, rapamycin treatment was discontinued. Since the age of 14 years the patient's superficial capillary malformations have been treated with pulsed dye laser (PDL) (10mm, 10ms, 6J/cm2), and the superficial venous malformations have been treated with multiplex neodymium-doped yttrium aluminum garnet (Nd:YAG) laser (PDL [10mm, 10ms, 6J/ cm2] followed after a 1-s delay by Nd:YAG laser [10mm, 15ms, 70J/cm2]) (Fig. 3A and B).
The phosphatidylinositol 3-kinase (PI3K/AKT)/phosphatase and tensin homolog(PTEN)/mammalian target of rapamycin (mTOR) pathway is implicated in the pathogenesis of hamartomatous syndromes such as TSC, vascular anomalies, overgrowth, and malignant tumors.2,4–6 mTOR, a kinase belonging to the phosphatidyl-3-inositol family, consists of 2 multiprotein complexes (mammalian target of rapamycin complex [mTORC]1 and mTORC2) and is involved in the regulation of multiple processes associated with growth, cell differentiation, angiogenesis, and modulation of the inflammatory response.7 The angiogenic activity of mTOR is mediated primarily via the translation and activation of hypoxia-inducible factor 1 (HIF-1), which in turn is implicated in VEGF expression in situations of cellular hypoxia and suppresses mTORC1 activity.7 The fact that TSC is one of the diseases most clearly associated with dysregulation of the mTOR pathway explains the appearance of different types of vascular malformations in this disease, although these alterations are rarely reported.2 Vascular anomalies described in TSC include angiomyolipomas, lymphatic malformations, and, less commonly, arterial anomalies (occlusion, stenosis, aneurysms), which are likely related to alterations of the vasa vasorum caused by hamartomas.2 Lymphedema in TSC8 may be the result of lymphatic malformations. It has been proposed that congenital and acquired lymphedema are more frequent in TSC.2
The involvement of an entire body segment, as in the present case, may be due to the loss of heterozygosity during early fetal development,2 combined with the germinal mutation. Postzygotic mosaic mutations that affect cell signaling pathways regulating cell growth, apoptosis, or migration can give rise to regional alterations, in some cases accompanied by overgrowth, which can compromise the skin, subcutaneous tissue, muscle, bone, and/or nerves. In terms of severity, overgrowth can be variable, stable, or progressive.9 When monitoring these patients, it should be borne in mind that alterations in these pathways can also increase the likelihood of developing various malignant tumors.2,4
In TSC patients, mTOR inhibitors such as rapamycin (sirolimus) have shown beneficial effects on neurological signs, but no clear effects on overgrowth and/or vascular malformations.2 Good results have been reported in other patients with vascular malformations.10 Further studies with better dose control and longer periods of administration are likely needed to determine its true efficacy. Blockade of the mTOR pathway could play a fundamental role in the development of vascular lesions in TSC patients.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Flores-Terry MÁ, Alegre-Sánchez A, Boixeda P, López-Gutiérrez JC. Complejo de esclerosis tuberosa asociado a hemihipertrofia y malformaciones vasculares combinadas. Actas Dermosifiliogr. 2019;110:164–167.