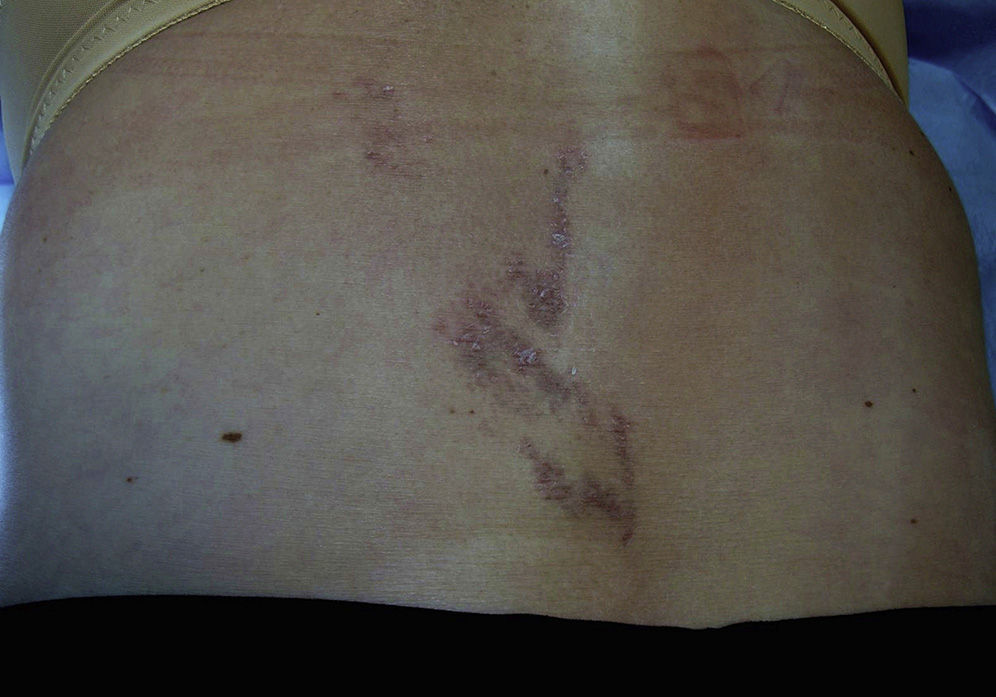
We report the case of a 63-year-old woman who presented a 3-month history of hyperpigmented and pruritic skin lesions in the lumbar region. Physical examination revealed violaceous-brown macules in a linear distribution with an italic S morphology (Fig. 1). The nails and mucosas were not affected. The patient did not report using systemic or topical treatments, exposure to the sun, or trauma prior to the onset of the lesions.
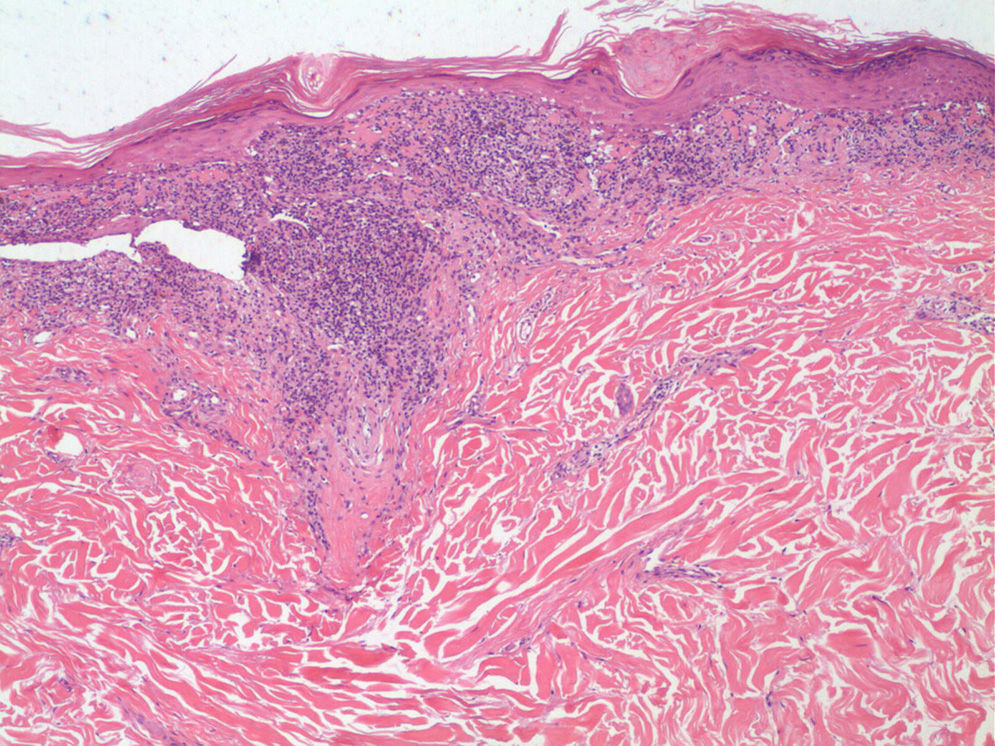
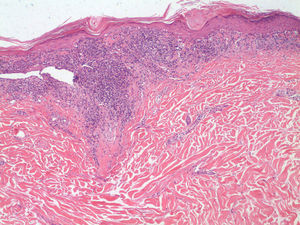
Dermoscopy revealed longitudinal pearly-white lines suggestive of Wickham striae (WS) and regressing brown macules in which there were grayish-brown dots and globules, some in a linear distribution following the outline of the WS or clustered in the depressed center of the WS (“ashy holes”) (Fig. 2). Skin biopsy revealed interface dermatitis with a lymphohistiocytic infiltrate, vacuolar degeneration of the basal layer, and apoptotic keratinocytes (Fig. 3).
Based on the clinical, dermoscopic, and histologic findings, we made a diagnosis of pigmented linear lichen planus (LLP). A course of oral antihistamines and topical corticosteroids was prescribed, daily for the first month followed by an alternating regimen for 3 months. This produced a gradual resolution of the lesions, which left a residual postinflammatory hyperpigmentation.
LLP is a condition of unknown etiology. It presents as hyperpigmented macules that usually arise in sun-exposed areas, but that are sometimes widespread.1 LLP differs clinically from classic lichen planus (LP) not only by the pigmentation, but also by its longer clinical course and the fact that the scalp, nails, and mucosas are not usually affected.1–5
One of the peculiarities of this case is the Blaschkoid distribution in an italic S shape. A review of the literature has revealed very few reports of LLP with isolated segmental manifestations, whether in a zosteriform distribution2 (in which case a history of herpes zoster must be sought, as this would suggest Wolf's isotopic phenomenon3) or following the Blaschko lines,4,5 or with overlapping segmental manifestations,3 in which linear lesions are associated with widespread nonsegmental lesions, indicative of diseases with a polygenic inheritance, including LP and other common dermatoses, such as psoriasis.6 However, with the exception of our patient, all affected individuals have been of Middle Eastern or South American origin1–5; our patient is the first reported case of LLP in a Caucasian woman. The differential diagnosis is broad and includes linear dermatoses such as lichen striatus, inflammatory linear verrucous epidermal nevus, linear and whorled nevoid hypermelanosis, and the segmental manifestations of ashy dermatosis.3,7 Differentiation from ashy dermatosis can be difficult and some authors even suggest that they are the same condition.7 In our case, the presence of pruritus, the absence of an erythematous border, and the histology and dermoscopy findings that included the presence of WS, led us to make a diagnosis of LLP.
We believe it is important to highlight the role of dermoscopy as a useful tool for diagnosis. Whitish striae or WS are the most significant dermoscopic pattern and are considered to be pathognomic of LP.8 Striae of different morphologies—round, arboriform, reticular, annular—have been described.8 The presence of pigmentation in the form of grayish-brown dots and globules has also been described; this can coexist with WS, outlining the lesions, or grouped within the central area of those with a round morphology (ashy holes).9 In more advanced stages, the WS may disappear, leaving only the pigmentation.9 Vázquez et al.10described 3 dermoscopic patterns in LLP: dots, diffuse, and mixed; those authors suggested that the more intense the granular deposits, the slower and more persistent the course of the disease, whereas a diffuse pattern of pigmentation with an absence of globules or dots was associated with earlier resolution.9,10 In our patient we observed a mottled pattern formed by clusters of numerous brown dots and globules and, as predicted, the course clinical was slow and the condition persisted for a year after diagnosis.
In conclusion, we have presented a rare case of LLP with a Blaschkoid distribution and we have described the most relevant dermoscopic features of this disease. Ever more cases like this one demonstrate the usefulness of dermoscopy not only in the diagnosis of inflammatory diseases of the skin, but also as a tool to predict the prognosis.
Please cite this article as: Baquero Sánchez E, Lorente-Lavirgen A, Domínguez Cruz J, Conejo-Mir J. Aportación de la dermatoscopia en el diagnóstico y pronóstico del liquen plano pigmentado lineal. Actas Dermosifiliogr. 2015;106:339–340.