Epidermolytic acanthoma (EA) is a rare benign lesion described by Shapiro and Baraf1 in 1970. It typically presents clinically as a solitary, asymptomatic verrucous papule. Histologically, there is an epidermal proliferation (acanthoma) with epidermolytic hyperkeratosis, without the concomitant presence of signs suggestive of other cutaneous tumors. The presence of multiple EAs in the genital and perigenital region is an individualized variant with well-defined clinical and pathologic characteristics.
A 49-year-old man with no past medical history of interest, reported the progressive appearance over the previous 18 months of multiple pruritic papules on his scrotum.
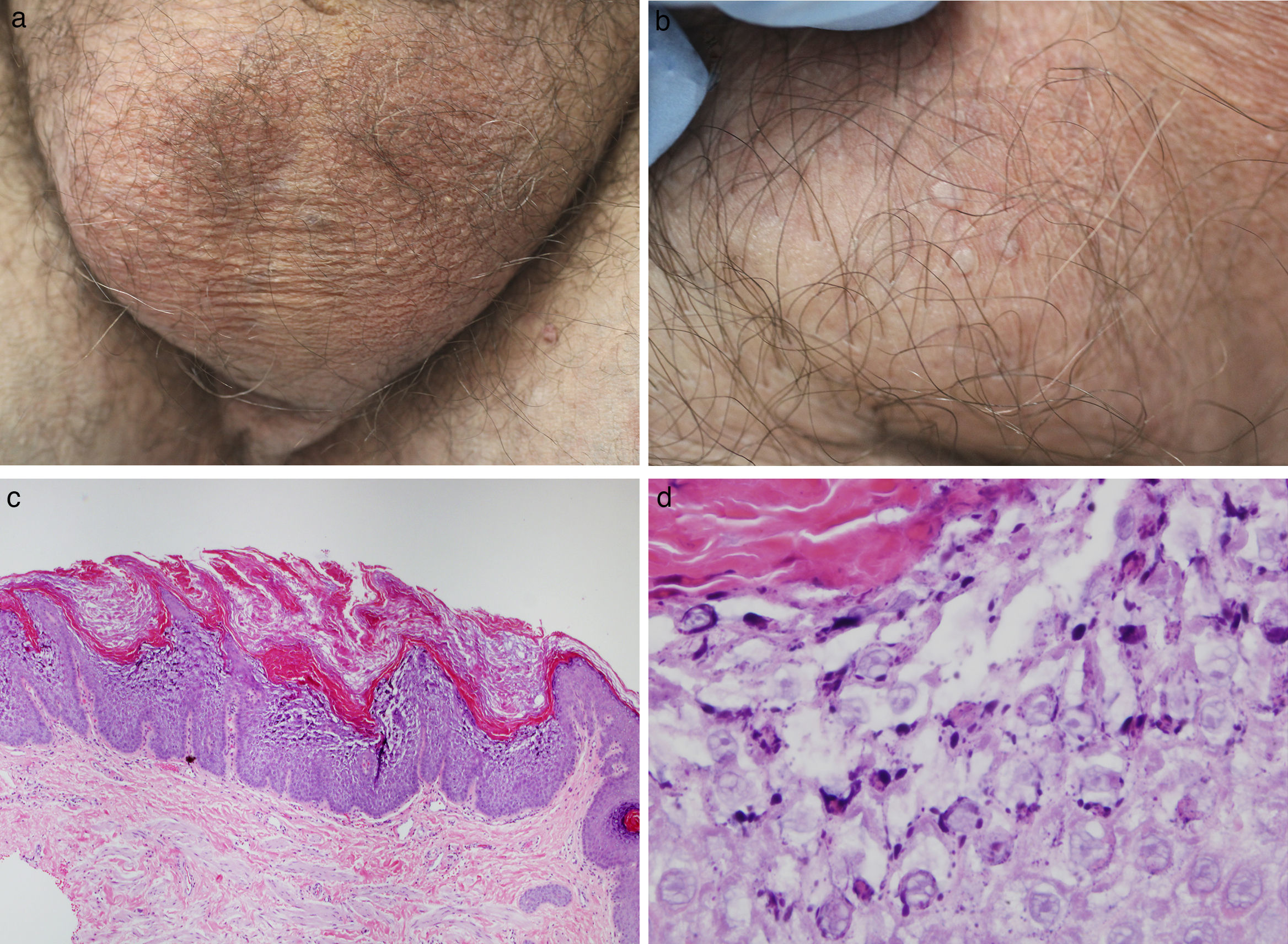
He denied any triggering factors such as trauma or high-risk sexual behavior. Physical examination revealed the presence of numerous, small (2-4mm), well-defined papules of whitish color and with a verrucous surface lying on a background of mild erythema (Fig. 1, A and B). Histology of one of the lesions showed an acanthotic epidermis with intense orthokeratotic hyperkeratosis with hypergranulosis and papillomatosis. Abundant large keratohyalin granules were observed in the stratum granulosum, associated with vacuolar cell degeneration and edema, giving rise to focal separation in the upper third of the epidermis (Fig. 1, C and D). No histopathological changes suggestive of human papillomavirus (HPV) infection were present, and immunohistochemistry with anti-HPV antibodies was negative.
A, Diffuse scrotal erythema and small, isolated papules. B, Detail of the lesions: multiple hyperkeratotic scrotal papules. C, Epidermolytic acanthoma: irregular acanthosis with orthokeratotic hyperkeratosis and papillomatosis. Hematoxylin and eosin (H&E), original magnification×40. D, Detail of the increased number of keratohyalin granules in the stratum granulosum and focal acantholysis. H&E, original magnification×400.
Treatment with 0.1% pimecrolimus cream was prescribed for the pruritus, and the lesions were then treated using cryotherapy, causing increased discomfort. A slight improvement was observed at the following visit, with reduced erythema and pruritus, and the lesions treated with cryotherapy had resolved.
EA is a benign and usually asymptomatic tumor that typically presents in adult individuals. It has been described as a solitary lesion, though occasionally it can present with multiple lesions that may be localized or widespread. The solitary forms can arise at any site, whereas multiple or widespread lesions appear to preferentially affect the genitocrural region.2
Clinically, multiple genital EA lesions present as numerous, flat or verrucous, skin-colored or whitish papules on the scrotum, vulva, perineum, or occasionally perianal region. The lesions can be asymptomatic or produce a variable degree of pruritus, causing scratching and persistence of the condition. The differential diagnosis includes other diseases more prevalent in the genital region, such as condyloma acuminatum, bowenoid papulosis, and molluscum contagiosum.3
Histologically there is a compact hyperkeratosis. Vacuolar degeneration of keratinocytes is observed in the granular layer and stratum spinosum of the epidermis, together with the presence of cytoplasmic amphophilic material and numerous basophilic bodies similar to keratohyalin and amorphous eosinophilic bodies of the trichohyalin type.4
The etiopathogenesis of EA is unknown. Some potential triggers have been identified, including viral infections, UV exposure, immunosuppression, and recurrent trauma (scratching).5–7 Mutations in the keratin K1 and K10 genes have been reported in isolated cases, and there has been no evidence of the presence or participation of HPV in the majority of cases studied.8,9
Multiple asymptomatic EA does not require treatment. However, certain topical keratolytic treatments (lactic, salicylic, or glycolic acid) have been found to be effective in some cases, as have more aggressive treatments, such as curettage, cryotherapy, and carbon dioxide laser. Low-potency topical corticosteroids can be useful in cases with pruritus, and the use of calcineurin inhibitors has also recently been described.10
Multiple anogenital EA is a clinical variant of EA that can present with persistent genital pruritus and must be included in the differential diagnosis of multiple papular genital lesions. The characteristic histological findings of EA make skin biopsy useful to confirm the diagnosis.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: García-Martínez P, Curto-Barredo L, Rovira-López R, Pujol RM. Acantomas epidermolíticos múltiples del escroto: lo que el prurito genital puede esconder. Actas Dermosifiliogr. 2018;109:81–82.