Warts are among the most common skin infections in children. Although numerous treatment options are available, none are completely effective in a single session. Treatment is particularly complicated in children, not only because certain treatments are poorly tolerated, but also because parents frequently have unrealistic expectations. In this article, we offer an update on the treatments available for warts, focusing specifically on pediatric patients. We do not discuss treatments for oral and anogenital warts.
Las verrugas víricas son una de las infecciones cutáneas más frecuentes en los niños. Aunque existen múltiples opciones de tratamiento, no hay ningún tratamiento que garantice una total eficacia con una única sesión terapéutica. En la edad pediátrica el tratamiento es particularmente complicado, no solo porque algunos métodos son mal tolerados, sino también porque a menudo las expectativas de los padres respecto a la eficacia del tratamiento son poco realistas. Este artículo proporciona una actualización sobre las diferentes terapias antiverrugas, particularmente enfocado a los pacientes pediátricos, excluyendo el tratamiento de las verrugas de la mucosa oral y anogenital.
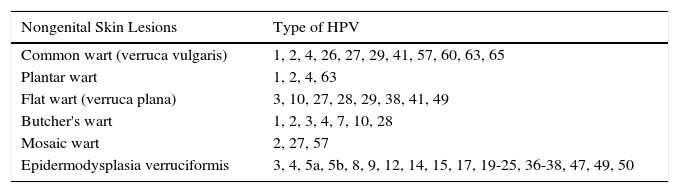
Human papillomavirus (HPV) is a DNA virus that belongs to the papillomavirus genus within the Papovaviridae family. There are at least 189 different strains of papillomavirus and 151 of these have been detected in human DNA (Table 1).1 HPV affects the skin and mucosa of humans, producing benign proliferations known as warts (Fig. 1). Some types of HPV have been associated with the development of malignant epithelial lesions in immunosuppressed patients or patients with anogenital warts, but this possibility is very rare during childhood.
Correlation Between Clinical Manifestations of Warts and Type of Human Papillomavirus (HPV).
| Nongenital Skin Lesions | Type of HPV |
|---|---|
| Common wart (verruca vulgaris) | 1, 2, 4, 26, 27, 29, 41, 57, 60, 63, 65 |
| Plantar wart | 1, 2, 4, 63 |
| Flat wart (verruca plana) | 3, 10, 27, 28, 29, 38, 41, 49 |
| Butcher's wart | 1, 2, 3, 4, 7, 10, 28 |
| Mosaic wart | 2, 27, 57 |
| Epidermodysplasia verruciformis | 3, 4, 5a, 5b, 8, 9, 12, 14, 15, 17, 19-25, 36-38, 47, 49, 50 |
According to data from family medicine registers in the United Kingdom and the Netherlands, the annual incidence of cutaneous warts is between 3 and 5 cases per 100 children aged between 5 and 14 years. The estimated prevalence in primary school children ranges from 4% to 33%, and between 9.1% and 21.7% of visits to the dermatologist are related to warts.2 Warts are transmitted directly through contact with infected skin or indirectly through contaminated surfaces. An affected family member or classmate has been identified as a risk factor for acquiring warts, even more so than the use of swimming pools or communal showers.3 The use of socks or other protective coverings to protect against the spread of infection in swimming pools has not been proven to be effective, and some authors have even indicated that it could stigmatize children and discourage them from going swimming altogether.4
The main goal when treating warts is to eradicate the lesions, while attempting to minimize pain, avoid scarring, and prevent recurrence. Choice of treatment will depend on the location, size, number, and type of warts, as well as on the age and level of cooperation of the patient. The experience of the treating physician may also have an influence.5
In this article, we provide an update on the treatments available for warts, with a specific focus on pediatric patients. We do not cover treatments for oral or anogenital warts.
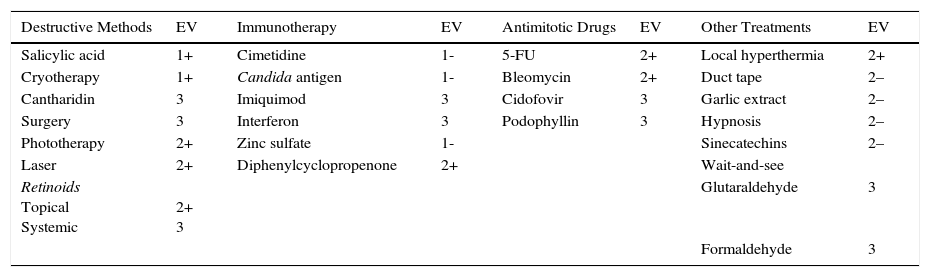
Types of Treatment AvailableThere are many types of treatment for warts (Table 2). The fact that so many treatments exist is indicative of their varying degrees of effectiveness, with success rates ranging between 32% and 93%.6,7
| Destructive Methods | EV | Immunotherapy | EV | Antimitotic Drugs | EV | Other Treatments | EV |
|---|---|---|---|---|---|---|---|
| Salicylic acid | 1+ | Cimetidine | 1- | 5-FU | 2+ | Local hyperthermia | 2+ |
| Cryotherapy | 1+ | Candida antigen | 1- | Bleomycin | 2+ | Duct tape | 2– |
| Cantharidin | 3 | Imiquimod | 3 | Cidofovir | 3 | Garlic extract | 2– |
| Surgery | 3 | Interferon | 3 | Podophyllin | 3 | Hypnosis | 2– |
| Phototherapy | 2+ | Zinc sulfate | 1- | Sinecatechins | 2– | ||
| Laser | 2+ | Diphenylcyclopropenone | 2+ | Wait-and-see | |||
| Retinoids Topical Systemic | 2+ 3 | Glutaraldehyde | 3 | ||||
| Formaldehyde | 3 |
Abbreviations: 5-FU, 5-flourouracil; EV, level of evidence.
1++ High-quality meta-analyses, systematic reviews of randomized controlled trials (RCTs) or, RCTs with a very low risk of bias; 1+ Well-conducted meta-analyses, systematic reviews of RCTs, or RCTs with a low risk of bias; 1–Meta-analyses, systematic reviews of RCTs, or RCTs with a high risk of bias; 2++ High-quality systematic reviews of case-control or cohort studies or high-quality case-control or cohort studies with a very low risk of confounding, bias, or chance and a high probability that the relationship is causal; 2+ Well-conducted case-control or cohort studies with a low risk of confounding, bias, or chance and a moderate probability that the relationship is causal; 2–Case-control or cohort studies with a high risk of confounding, bias, or chance and a significant risk that the relationship is not causal; 3 Nonanalytical studies (e.g., case reports, case series); 4 Expert opinion, formal consensus.
Destructive methods are those that cause nonspecific damage to infected keratinocytes and surrounding skin. Although these methods are associated with high recurrence, the fact that they are simple to use and relatively cheap explains why they are the most widely used treatments in routine practice.
Salicylic AcidSalicylic acid is a keratolytic agent that destroys the epidermis infected by the virus. It is available in different vehicles at concentrations of between 10% and 30%. Topical salicylic acid is still the treatment with the best evidence base and it is the only option approved by the US Food and Drug Administration for warts.8 It is therefore considered the treatment of choice. Approximately two-thirds of all warts clear within 3 to 6 months of treatment with topical salicylic acid.8 One systematic review of 6 randomized controlled trials comparing salicylic acid with placebo for the treatment of warts in adults and children reported cure rates of 75% and 48%, respectively.9 A Cochrane review of a meta-analysis of 6 studies with 486 participants showed statistically significant results in favor of the topical application of salicylic acid for warts in any location.10 Although no adverse effects have been reported (with the exception of local irritation), in one study that compared 60% salicylic acid and monochloroacetic acid versus placebo, a patient developed cellulitis in the treated area.11
CryotherapyCryotherapy consists of freezing the wart with liquid nitrogen for 10 to 20seconds every 2 to 3 weeks. Although the exact mechanism of action is unknown, the freezing is thought to cause local irritation, thereby stimulating an immune response. One multicenter clinical trial found no significant differences between the efficacy of cryotherapy with liquid nitrogen and 50% salicylic acid in patients with plantar warts. The fact that cryotherapy is more expensive, however, would appear to tip the balance in favor of salicylic acid.12 Another randomized controlled trial compared the efficacy of cryotherapy, salicylic acid, and a wait-and-see approach for common and plantar warts. The authors found that cryotherapy was more effective for nonplantar warts, but observed no clinically significant differences after 13 weeks of treatment. Finally, patients treated with cryotherapy experienced more adverse effects than those in the other 2 groups.13 Some authors are of the opinion that cryotherapy should not be used for longer than 3 months or for more than 4 procedures, as there is no evidence of any benefit of continuing treatment for longer, particularly in the case of warts on the hands and feet.14 The main disadvantage of cryotherapy is that the procedure can be painful and cause blistering; there is also a risk of residual scarring, hyperpigmentation, and hypopigmentation (Fig. 2).
CantharidinCantharidin is a blistering agent produced by beetles of the order Meloidae Coleoptera. It is used at a concentration of 0.7% or 1% and once applied should be covered with an occlusive dressing for 24hours. Cure rates of over 80% have been reported for common, plantar, and periungual warts.15 Although the application of cantharidin itself is not painful, the resulting blistering may be accompanied by erythema, pain, pruritus, and postinflammatory hyperpigmentation. More severe though less frequent adverse effects have been described, such as lymphangitis, bacterial cellulitis, and scarring.16
SurgerySurgical treatment of warts involves the radical eradication of lesions by conventional surgery, electrosurgery, or curettage. One of the advantages of surgery is that it provides a rapid solution and can therefore be beneficial in the case of recalcitrant or isolated warts. It is, however, associated with high rates of bleeding, scarring, and bacterial infections, and estimated recurrence is around 20%.17 One study showed a higher overall clearance rate for curettage and electrodesiccation (94%) than for podophyllin (41%) or cryotherapy (79%). Recurrence rates, however, were similar for the 3 treatments.17
ElectrocoagulationElectrocoagulation causes heat-induced tissue destruction. Although it is very useful for treating filiform or small isolated warts, it is not a mainstay treatment for children,18 as it requires the use of local anesthesia and can leave a scar.
PhototherapyPhototherapy causes direct tissue destruction through exposure to different light sources. It is a painful procedure that is not available at all hospitals. As such it is not considered a first-line option for pediatric patients.
Photodynamic TherapyThe mechanism of action of photodynamic therapy is tissue destruction secondary to an inflammatory response induced by a phototoxic reaction. The recommended procedure involves applying 5-aminolevulinic acid 20% cream on the wart and covering this with an occlusive polyurethane dressing for 4hours. The wart is then irradiated for 20minutes with a light source with a wavelength of between 590 and 700nm and an irradiance of 50mW/cm2.19 One study of photodynamic therapy with white light and 5-aminolevulinic acid combined with keratolytics in patients with refractory palmar and plantar warts reported a cure rate of 56% for treated warts after 18 weeks of treatment.20 Adverse reactions are typically local and include erythema, a burning sensation, and pain. Because the procedure is painful and is additionally not approved for warts, it is not recommended in children.
Laser TherapyCarbon dioxide (CO2) laser–induced destruction of wart tissue has been used for some time to treat viral warts.21 Its use is not justified in pediatric patients as it is painful and can cause scarring.22 Pulsed-dye laser therapy causes direct microvascular damage within the warts. Its mechanism of action is based on localized tissue necrosis secondary to the absorption of energy by components of the capillaries. It is well tolerated by children. Two large cohort studies reported complete resolution rates of 48% for warts and 75% for children with palmar-plantar warts.23 Pulsed-dye lasers can also cause pain and scarring, but less so than CO2 lasers. Adverse reactions described for pulsed-dye laser therapy include crusting, petechiae, and purpura.24
GlutaraldehydeGlutaraldehyde is an antiviral agent. A 10% or 20% solution is applied daily over a period of 3 months.23 A cure rate of 72% was reported in a series of 25 patients with recalcitrant warts.23 There have been reports of deep necrosis after repeated application23 and of contact dermatitis.25
FormaldehydeFormaldehyde, another antiviral agent, is applied once daily in a 0.7% gel or at a concentration of 3% to 10% in solution. One open-label study of 646 children treated with formaldehyde reported a cure rate of 80%.23 The substance is allergenic and can cause contact sensitization.
RetinoidsRetinoids are vitamin A derivatives (retinol) with cellular and biologic actions that include regulation of epidermal proliferation and differentiation. They are used both systemically—acitretin at a dose of 0.5 to 1mg/kg/d for a maximum of 3 months—and topically—tretinoin 0.05% applied once daily.23 In one observational study, 80% of children (16/20) treated with oral etretinate for 3 months achieved total wart clearance.18 In a case-control study of 50 children treated with tretinoin 0.05% or nothing, those who received the treatment achieved a clearance rate of 85%, compared with a 32% rate in the control group.26 Tretinoin 0.05% is a good option for flat facial warts.18 However, considering the caution that must be applied when using oral retinoids, particularly in teenage girls, and the fact that there is little evidence on their efficacy, etretinate is not recommended in children.18
ImmunotherapyImmunotherapy drugs are used to elicit humoral and/or cellular immune responses and thereby eliminate the viral infection responsible for warts.
CimetidineOral cimetidine is an H2 blocker that acts as a T cell–immunomodulator. It appears to inhibit suppressor lymphocyte function, thereby enhancing T-cell immunity.27 Cimetidine is administered orally at daily doses of 20 to 40mg/d, with a maximum dose of 600mg per day. One double-blind study found no statistically significant differences between oral cimetidine 400mg administered 3 times a day for 12 weeks and placebo for warts in patients aged over 12 years, while another randomized trial found no differences between cimetidine 40mg/kg/d versus placebo in women and children aged between 4 and 39 years.8 Gastrointestinal complaints such as nausea and epigastralgia were the most common adverse effects described.28
Candida AntigenCandida antigen is a substance derived from purified extracts of Candida albicans. It is typically injected intralesionally, either pure or diluted to a concentration of 50% in lidocaine. The dose is 0.2 to 0.3mL and at least 3 applications—separated by 3 weeks—are required.29,30 Intralesional injections induce a localized HPV-specific cell-mediated response that targets both the injected wart and warts located at a distance. In a recent Spanish study of Candida antigen immunotherapy in 220 children, after a mean of 2.73 intralesional injections, 70.9% of children achieved complete resolution, 16.8% achieved partial resolution, and 12.2% did not respond.29 Of particular note was that the fact that over half of the patients with multiple lesions achieved complete resolution of lesions located at a distance, i.e., lesions that had not been directly treated. In a study of 100 patients of all ages at the Mayo Clinic, 80% of patients responded to treatment, with 39% achieving complete response and 41% achieving partial response.30
Candida antigen immunotherapy is normally well tolerated and does not leave sequelae,29,30 although there have been reports of pain, swelling, and purple discoloration in distal fingertips in the case of subungual warts 24hours after the injection; the effects disappeared, without sequelae.31 There has also been a report of vitiligo at the injection site of Candida antigen in an 8-year-old girl.32
ImiquimodThe exact mechanism of action of imiquimod is unknown, but it is assumed to involve stimulation of both innate and cell-mediated immunity.33 In one study of recalcitrant subungual and periungual warts, 80% of patients treated with a preparation of salicylic acid followed by imiquimod 5% cream with an occlusive dressing 5 times a week for 16 weeks achieved complete resolution. The most common adverse reactions were local erythema, pruritus, and a burning sensation.34
InterferonIntralesional interferon is approved for the treatment of anogenital warts caused by HPV in adults, but it is not recommended for children due to its high toxicity and the limited experience with its use.22
Zinc SulfateZinc sulfate appears to act as an immunomodulating agent via the polyclonal activation of lymphocytes. It is used at a dose of 10mg/kg/d to treat warts. One comparative double-blind study found that zinc sulfate 10mg/kg/d appeared to be more efficacious than cimetidine in children and adults with multiple or recalcitrant warts. However, given the few patients analyzed, no definitive conclusions can be drawn regarding the efficacy of zinc sulfate for the treatment of warts.28
DiphenylcyclopropenoneDiphenylcyclopropenone is an allergic contact sensitizer used to treat resistant warts. Initial sensitization is required. To achieve this, diphenylcyclopropenone 2% is applied to a 1-cm2 area and covered for 48hours. The actual treatment consists of applying diphenylcyclopropenone 1% to the affected warts (or 2% for plantar warts) and covering these for 8hours. The process is repeated at intervals of 1 to 4 weeks.35 One retrospective study analyzed the 3-weekly application of diphenylcyclopropenone at concentrations of 0.5% to 5% in 25 patients (including adolescents) with recalcitrant warts. Fourteen patients (56%) achieved complete resolution after a mean of 4 cycles, while the remaining patients (44%) showed no improvement.36 Adverse effects are uncommon, but there have been reports of blisters, urticaria, and exacerbation of atopic dermatitis.35,36
Antimitotic Drugs5-Fluorouracil5-fluorouracil is a fluorinated pyrimidine that is effective against viral warts because it blocks DNA and RNA synthesis of viral particles and reduces epidermal proliferation.37 It can be applied topically, with daily applications, or injected into the lesion with local anesthesia. Although several studies have shown it to be effective,37 it has not been tested in children.18 The most common adverse effects observed with both topical and systemic 5-fluorouracil are local irritation, moderate to severe pain during application, blistering, and onycholysis in periungual lesions.10
BleomycinBleomycin has antibacterial, antiviral, and cytotoxic activity, and by blocking cellular and viral DNA synthesis, it causes acute tissue necrosis that stimulates an immune response.8 It is injected intralesionally at concentrations of between 0.25% and 1%. Bleomycin causes pain, erythema, and inflammation during the procedure and up to a week afterwards. Widely varying cure rates (in the range of 16% to 94%) have been reported for the treatment of warts and results must therefore be interpreted with caution.38 Two placebo-controlled studies reported that intralesional bleomycin was not effective.10 The resulting necrosis causes ulcers, scarring, residual hyperpigmentation, and nail changes.39 There has been a report of flagellated hyperpigmentation in a 31-year-old woman with a recalcitrant plantar wart treated with intralesional bleomycin.40 Intralesional bleomycin has not been extensively studied in the pediatric population and should therefore be avoided in young children.18
CidofovirCidofovir is an antiviral agent that acts via competitive inhibition of viral polymerase DNA. It is applied as a topical cream at a concentration of 1% or 3%. It has been found to be useful for resistant warts that do not respond to standard treatments.41 In one series of 7 children with warts on their hands and feet, treatment with topical cidofovir 1% applied once daily for 12 weeks resulted in complete resolution in 4 patients. However, further studies with more patients are needed to demonstrate the efficacy and safety of topical cidofovir in children.18
PodophyllinPodophyllin is an antimitotic agent derived from the plant Podophyllum peltatum. It is used at a concentration of between 10% and 25% in alcohol or benzoin, and causes tissue necrosis. It must be left on the affected area for between 1 to 4hours, and then removed. It is reapplied weekly for up to 6 weeks.17 Podophyllin has been successfully used to treat anogenital warts, but in a study of 382 adults and children, it was found to be equivalent to salicylic acid for the treatment of plantar warts.42 Nevertheless, because it has been associated with neurotoxicity and myelotoxicity, it is not recommended for pediatric patients.18
Other TreatmentsA range of other treatments have proven effective for the treatment of multiple and/or recalcitrant warts in studies with low statistical power. Despite the poor scientific evidence on their effectiveness, however, these treatments tend to be accepted by parents, carers, and patients, as they are considered “natural” and do not cause pain or adverse effects.
Local HyperthermiaLocal hyperthermia is a simple treatment, particularly for multiple lesions. The affected area is soaked in water at a temperature of between 44°C and 47°C for 30minutes once a day for 3 consecutive days. This process is repeated 2 weeks later. Although the exact mechanism of action involved is not known, some authors have suggested that the local heat might trigger the death of HPV-infected keratinocytes.43 The same authors observed that hyperthermia caused the migration of mature Langerhans cells, stimulating a specific immune system response against infected keratinocytes. No serious adverse effects have been reported, although patients may experience a burning sensation and local erythema.
Duct TapeThe mechanism of action underlying the use of duct tape to treat warts is not known, but like other treatments, it would appear to involve the stimulation of the immune system in response to local irritation. The wart is covered with duct tape (or a plaster) for 6 days, after which it is soaked in water, pared down, and left uncovered for 12hours. The cycle is repeated until the wart disappears. One prospective study that compared the effectiveness of duct tape versus standard local cryotherapy to treat warts in pediatric patients reported that duct tape occlusion was significantly more efficacious than cryotherapy. Of the 26 children who received this treatment, 22 (85%) achieved complete resolution of warts compared with 15 (60%) of the 25 children treated with cryotherapy (P=.05).6 These high cure rates, however, should be viewed with caution considering the absence of well-designed studies with large samples.
Sinecatechins (Polyphenon E)Polyphenon E is a green tea leaf extract (Camellia sinensis) that appears to induce cell cycle arrest, activate apoptosis, inhibit HPV transcription, and stimulate cell-mediated immunity. The combination of these actions results in the eradication of both clinical and subclinical HPV-infected cells. Polyphenon E is available as an ointment (15%) and is applied 3 times a week for a maximum of 16 weeks.20
Garlic ExtractsVarious components of garlic (Allium sativum) have been shown to have antiviral activity and to inhibit the proliferation of HPV-infected cells. In one placebo-controlled study, the application of garlic extracts resulted in complete resolution of warts, without recurrence after 3 to 4 months.8
HypnosisHypnosis has been used to treat warts in children and adults for years. It is believed to stimulate the immune system, leading to the resolution of lesions. No studies, however, have determined whether the warts heal because of hypnosis or simply because of spontaneous regression.8
Wait-and-SeeIt has been calculated that warts resolve spontaneously within 2 years in approximately two-thirds of patients,8 and hence many dermatologists prefer to adopt a watch-and-see approach rather than prescribe an active treatment. Such an approach, however, is not always possible as lesions can become ugly and cause stigmatization, leading many parents and/or patients to opt for treatment.
Our ApproachSalicylic acid in petrolatum is our treatment of choice for young children with large, multiple, or periungual warts. Preparations containing high concentrations of salicylic acid (25%-40%) are particularly effective as keratolytic agents, but it is important to explain the application process carefully and to ensure adherence to treatment. We tend to use concentrations of between 25% and 35%. The product is applied once a day and the surrounding area is protected with pure petrolatum. Both areas are then covered with plastic overnight. This process is repeated for several consecutive days. The hyperkeratotic surface is pared down before each application, ideally after a bath or shower. If the wart persists or returns, the process can be repeated as many times as necessary.
Many parents request cryotherapy as they consider it to be more practical than the daily application of a keratolytic. Cryotherapy is fast and simple, but it tends to be poorly tolerated by younger patients and we believe that it is thus reasonable to first try to eradicate the lesion with a topical keratolytic, unless it is located on the face. Cryotherapy is also not our first choice for large or multiple lesions, or for periungual lesions due to the risk of irreversible postinflammatory onychodystrophy. Another factor to take into account is that cryotherapy requires frequent visits to the hospital, leading to possible absences from school or work.
Although cantharidin is the least used destructive method in our practice, we do consider it to be a useful option. Its main disadvantage is that it is not sold in Spain, and furthermore it has to be applied by health care staff, meaning more hospital visits. Use of a color additive can help to identify treated areas in patients with extensive lesions.
Curettage and electrodessication, with local anesthesia, is useful for filiform warts on the face. While effective, this method requires the patient to remain still, which is frequently a problem with young patients. In such cases sedation may be contemplated. The procedure is even simpler when the base of the wart is very small, as electrodessication tends to be unnecessary.
Intralesional Candida antigen immunotherapy offers good results for recalcitrant, large, and periungual warts. However, because the substance is not approved for this indication, it can be difficult to obtain in certain centers. We have occasionally observed regression of recalcitrant lesions with cimetidine and duct tape, although in such cases, it is difficult to identify the true reason for the cure.
ConclusionsTreatment of warts is frequently frustrating for doctors, patients, and carers as there is no perfect treatment, i.e., there is no one treatment that is fast, painless, highly effective, and associated with a low risk of recurrence. Many treatment options therefore exist and the choice of one or another will depend on the number of warts, their location, their size, the age of the patient, and the experience of the dermatologist. Whatever treatment is chosen, it is important to clearly explain to parents or carers that warts are benign and tend to resolve spontaneously, while at the same time establishing realistic expectations about treatment outcomes.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Gerlero P, Hernández-Martín Á. Actualización sobre el tratamiento de las verrugas vulgares en los niños. Actas Dermosifiliogr. 2016;107:551–558.